Infection Control Technologies: A Primer and Provider Selection Guide
Home » Infection Control Technologies: A Primer and Provider Selection Guide
Home » Infection Control Technologies: A Primer and Provider Selection Guide
Content
1. Purpose of White Paper
The purpose of this paper is to help LeadingAge and other aging services organizations understand the range of infection control technologies available in the marketplace, their uses, and their benefits.
In addition, the white paper will help providers plan for, select, and implement an infection control solution. Complementary LeadingAge CAST tools—including an online selection tool, a matrix of infection control technology solutions, case studies, and the LeadingAge Member Community—can help providers select the technologies that best fit their requirements.
Disclaimers: This information is meant to assist in understanding infection control technologies but cannot possibly include all systems that may be available. Products mentioned in this report are only illustrative examples and have not been tested or independently evaluated or endorsed by LeadingAge or LeadingAge CAST. Please use this information as a general guideline in understanding functionalities and examples of current infection control systems. Where appropriate, provider case studies were identified.
1.2 Executive Summary
This white paper presents the range of infection control technologies available, their uses, and their benefits. Aging services providers can use it to plan for, select, and implement an infection control solution. Several additional LeadingAge CAST tools complement the white paper to help providers choose the technologies on the marketplace that are the best fit for their organizations:
- The CAST Infection Control Online Selection Tool to narrow down the selection to a few shortlisted candidate systems and vendors that meet the must-have high-level requirements.
- The CAST Infection Control Technology Selection Matrix, which outlines many additional options and detailed features and functionalities to further narrow the shortlisted products to a list of two or three vendors who can be invited to submit a response to a request for proposals.
- Case studies collected by CAST, to help review potential vendors.
- LeadingAge Member Community is a resource to ask peers about the shortlisted products and their experience with these vendors.
Why Infection Control Matters
In the United States alone, more than 15,000 long-term care (LTC) facilities serve more than 1 million residents. The residents and staff in LTC facilities have an increased risk of infection due to the unique challenges in the care setting and the resident population. Infections associated with health care account for as many as 380,000 deaths annually.
Infections associated with health care account for as many as 380,000 deaths annually.
Infections also increase health care costs and may result in hospitalization. For these reasons, all staff in LTC facilities must work together to reduce infections and provide safe care for residents and a safe work environment for staff. One way is through use of infection control technologies.
Types of Infection Control Technologies
Infection control technologies are varied and may include equipment such as cleaning chambers or robotic floor scrubbers. Ultraviolet (UV) technology offers a nonchemical approach to disinfection. Air filtration and disinfection can be important elements of infection control. This white paper reviews several air solutions and concludes that advanced air purification technology (AAPT), an in-duct system, provides the most comprehensive air purification available.
Infection surveillance, control, and reporting software solutions are designed to help health care facilities track and control the spread of infectious diseases. Technology can simplify the process of capturing health screening data, through use of a digital sign-in/kiosk system or similar method, to identify people who may be infected. Technology can also support contact tracing, to help providers identify people who may have been or are confirmed to have been exposed to an infectious disease.
Infection surveillance, control, and reporting software solutions can help health care facilities track and control the spread of infectious diseases.
Electronic Health Records (EHRs)/Electronic Medical Records (EMRs) can be used as decision-support tools, helping guide clinicians to make decisions to prevent facility-acquired infections (FAIs). EHRs/EMRs can also offer predictive modeling via machine learning, aiding clinicians and infection programs in targeting patients at greatest risk of developing an FAI.
Benefits of Infection Control Technologies
Benefits of reducing FAIs include increasing residents’ quality of care and quality of life and increasing resident and family satisfaction. Fewer infections lowers operational and health care costs, reduces staff sick leave and increases staff efficiencies and satisfaction, improves public health and reporting capabilities, mitigates the community’s risks and liabilities, and improves the community’s reputation.
Several kinds of LTPAC provider business models can support technology investments.
Provider Business Models
Long-term and post-acute care (LTPAC) provider business models that could support technology investments include grants and innovative funding vehicles, including the Provider Relief Fund (part of the CARES Act), Commercial Property-Assessed Clean Energy (C-PACE), and Civil Money Penalty Funds (CMP). Potential Affordable Care Act (ACA) opportunities include new care delivery and payment models that could give LTPAC providers using certain technologies the opportunity to derive revenues from strategic partners.
Infection control technologies deliver potential financial savings to various stakeholders. Return on investment (ROI) can accrue to patients and/or their families, to payers, and to care providers, including LTPAC providers, physician group accountable care organizations, and hospitals. However, the financial savings and ROI depend on a number of factors, including the care/service delivery model, the payment/reimbursement model, the technology, and costs. The white paper outlines how to calculate ROI.
Planning for and Selecting Appropriate Infection Control Technology
Planning and choosing the technology that best fits each environment’s unique needs, and supports the organization’s overall infection control program and infrastructure, is crucial. Proactively assessing the needs of residents, staff, and family members is an important first step.
Proactively assessing the needs of residents, staff, and family members is an important first step.
Many elements should play a role in choosing infection control technology. Visioning and strategic planning are important, as is conducting an organizational readiness assessment. Consider physical and IT infrastructure, available technology solutions, data availability and needs, interoperability/interfacing capability, resident/client and family needs, staff needs and competencies and availability, and partner assessments.
2. Infection Control
2.1 Definition
Infection control refers to the policy and procedures implemented to control and minimize the dissemination of infections in hospitals and other health care settings with the main purpose of reducing infection rates.
2.1.1 History of Infection Control
Infection control as a formal entity was established in the early 1950s in the United States. By the late 1950s and 1960s, a small number of hospitals began to recognize healthcare-associated infections and implemented some infection control concepts. They focused on monitoring patients for these infections and incorporated the basic understandings of epidemiology to make sure that people understood the risk factors for infections.
However, most of the infection control programs were organized and managed by large academic centers rather than public health agencies, which led to sporadic efficiency and suboptimal outcomes.
A new era in infection control began less than 25 years ago.
A new era in infection control began less than 25 years ago, with three pivotal events. In 1999, the Institute of Medicine issued a report highlighting the large number of preventable errors in health care, and in 2002 the Chicago Tribune reported on substantial numbers of preventable and deadly hospital-acquired infections. From 2004 to 2006, publications announced that standardization of central venous catheter insertion process brought significant reductions in bloodstream infection rates.
2.2.2 Today’s Approach
Now, consumers demand more transparency and accountability, increased scrutiny and regulation, and rapid reductions in facility-acquired infection (FAI) rates.
The role of infection control is to prevent and reduce the risk for facility-acquired infections.
Infection control programs can achieve this goal through surveillance, isolation, outbreak management, environmental hygiene, employee health, education, and infections prevention policies and management.[i]
The role of infection control is to prevent and reduce the risk for facility-acquired infections.
Two tiers of recommended precautions can prevent the spread of infections in health care settings:[ii]
- Standard Precautions: Standard precautions are used for all patient care. Based on a risk assessment, they make use of common sense practices and personal protective equipment (PPE) that protects health care providers from becoming infected and spreading infection from patient to patient.
- Transmission-Based Precautions: Transmission-based precautions are the second tier of basic infection control. These additional precautions are used with standard precautions for patients who may be infected or colonized with certain infectious agents in order to prevent infection transmission.
Source: Guideline for Isolation Precautions
2.2 Importance/Relevance
In the United States alone, more than 15,000 long-term care (LTC) facilities serve more than 1 million residents. The residents and staff in LTC facilities have an increased risk of infection due to the unique challenges in the care setting and the resident population. Infections associated with health care account for as many as 380,000 deaths annually. Additionally, infections increase health care costs and may result in hospitalization. For these reasons, all staff in LTC facilities must work together to reduce infections and provide safe care for residents and a safe work environment for staff.[iii]
Before COVID-19, most LTC staff had never dealt with a novel infectious disease outbreak.
Before COVID-19, most LTC staff had never dealt with a novel infectious disease outbreak. The 2009 H1N1 influenza pandemic primarily affected children and young adults, and by August 10, 2010, the World Health Organization declared an end to the pandemic.
Prior to COVID-19, antiviral chemoprophylaxis, adaptable vaccines, and quick implementation of infection control measures such as isolation and PPE use effectively halted outbreaks. The 2009 H1N1 was the last time N95 masks were needed in most nursing homes.
When the SARS-CoV-2 virus entered our country in 2020, the entire nursing home industry was jolted into the unknown. It could either adapt and overcome or succumb.[iv]
3 Types and Uses of Infection Control Technologies (non-mutually exclusive categories):
3.1 Hand Hygiene Compliance
According to the U.S. Centers for Disease Control and Prevention (CDC), regular handwashing is one of the best ways to remove germs, avoid getting sick, and prevent the spread of germs to others. Whether at home, at work, traveling, or out in the community, handwashing with soap and water can protect people and their families.[v]
Feces from people or animals are an important source of germs like Salmonella, E. coli O157, and norovirus that cause diarrhea, and feces can spread some respiratory infections like adenovirus and hand-foot-mouth disease. These kinds of germs can get onto hands after people use the toilet or change a diaper. They can also spread in less obvious ways, like after handling raw meats that have invisible amounts of animal feces on them.
A single gram of human feces—which is about the weight of a paper clip—can contain one trillion germs. Germs can also get onto hands if people touch any object that has germs on it because someone coughed or sneezed on it or another contaminated object touched it. When these germs get onto hands and are not washed off, they can be passed from person to person and make people sick.[vi]
Handwashing helps prevent infections in many ways.
Handwashing with soap removes germs from hands. Handwashing helps prevent infections because of the following reasons:
- People frequently touch their eyes, nose, and mouth without even realizing it. Germs can get into the body through the eyes, nose, and mouth and make us sick.
- Germs from unwashed hands can get into foods and drinks while people prepare or consume them. Germs can multiply in some types of foods or drinks, under certain conditions, and make people sick.
- Germs from unwashed hands can be transferred to other objects, like handrails, tabletops, or toys, and then transferred to another person’s hands.
- Removing germs through handwashing helps prevent diarrhea and respiratory infections and may even help prevent skin and eye infections.
Teaching people about handwashing helps them and their communities stay healthy. Handwashing education in the community accomplishes the following:
- Reduces the number of people who get sick with diarrhea by 23-40%.
- Reduces diarrheal illness in people with weakened immune systems by 58%.
- Reduces respiratory illnesses, like colds, in the general population by 16-21%.
- Reduces absenteeism due to gastrointestinal illness in schoolchildren by 29-57%.
The World Health Organization (WHO) guidelines on hand hygiene push for new innovations and technologies to be developed to better measure hand hygiene practices. Sensing technology is an emerging evidence-based strategy to measure and promote hand hygiene. Hygiene-specific sensing technology is designed to ensure health care workers perform hand hygiene during WHO’s Five Moments for Hand Hygiene (critical moments of care). The technology increases accountability, provides a monitoring system, and creates an overall sense of ownership among health care workers.
The technology can record and promote hand hygiene compliance using a special badge with colored lights to indicate hand hygiene status. Green means hand hygiene has been performed, yellow is a reminder to clean hands, and red means hand hygiene should occur immediately.
The image below shows how the technology works. A sensor in the badge automatically communicates with transmitters at key points in a patient’s room (such as the room entrance/exit and patient bedside), detecting each hand hygiene opportunity.
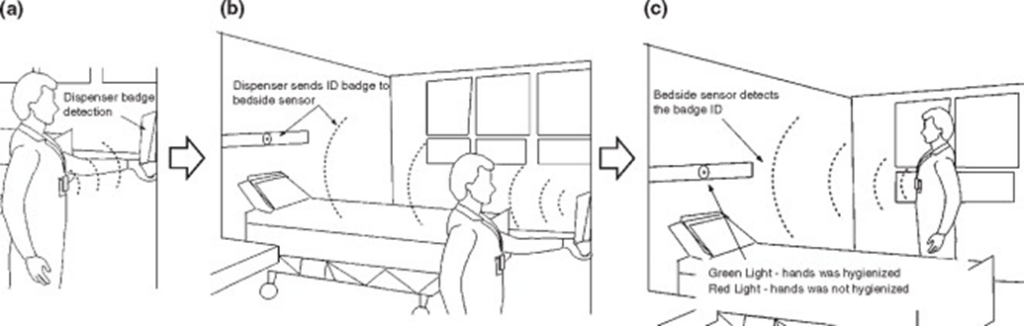
Direct observation, when someone watches in person or on video, has long been considered the gold standard for measuring hand hygiene compliance because it provides the most information. However, it tends to be labor intensive and costly. Direct observation also has limitations with validity, including reliability, sampling bias, and patient privacy concerns. Sensing technology, on the other hand, may be a superior alternative to direct observation that addresses these limitations.
According to findings from Grenado-Villar et al., using sensing technology is a more comprehensive way than direct observation to measure the proportion of hand hygiene opportunities caregivers take. While there are some limitations to sensing technology, such as lack of context-specific data,[vii] sensing technology can provide real-time analysis and feedback on hand hygiene activities.[viii]
Monitoring the Patient Zone using technology is another strategy to measure hand hygiene.
Monitoring the Patient Zone using technology is another strategy to measure hand hygiene. The Patient Zone is an electronically monitored zone set up around the resident’s bed to detect every hand hygiene opportunity. A caregiver may enter the room wearing a badge that prompts them to wash or sanitize their hands before entering the Patient Zone.
The bed kit creates a zone around the resident. Once washing/sanitizing is completed, the caregiver can approach the resident and interact with them in the Patient Zone. The caregiver must wash or sanitize after leaving the Patient Zone. The information from the badge, dispenser, and bed kits is sent to a dashboard, which reports all the data.
3.2 Surface/Object Cleaning and Disinfection
3.2.1 Cleaning
Cleaning is the removal of foreign material such as soil and organic material from objects and is normally accomplished using water with soap/detergents or enzymatic products. Thorough cleaning is required before high-level disinfection and sterilization because inorganic and organic materials that remain on instrument surfaces interfere with the effectiveness of these processes.
Also, if soiled materials dry or bake onto the instruments, the removal process becomes more difficult and the disinfection or sterilization process less effective or ineffective. Surgical instruments should be presoaked or rinsed to prevent drying of blood and to soften or remove blood from the instruments.
Various technologies can assist with cleaning.
Cleaning is done manually in use areas without mechanical units such as ultrasonic cleaners or washer-disinfectors or for fragile or difficult-to-clean instruments. With manual cleaning, the two essential components are friction and fluidics.
- Friction: Rubbing/scrubbing the soiled area with a brush is an old and dependable method.
- Fluidics: Fluids under pressure can remove soil and debris from internal channels after brushing and when the design does not allow a brush to pass through a channel.
When a washer-disinfector is used, care should be taken in loading instruments. Hinged instruments should be opened fully to allow adequate contact with the detergent solution. Instruments should not be stacked in washers, and instruments should be disassembled as much as possible.[ix]
Various technologies can assist with cleaning. For example, many human-operated cleaning technologies exist, including large walk-behind floor scrubbers or handheld cleaning devices. A cleaning chamber may also be used to clean surfaces of mobile devices or other small objects. For example, a cell phone may be placed in a case/chamber with UV light to clean and sanitize it. Robotic cleaning technologies can help eliminate the need for staff to operate the technology. For example, a robotic floor scrubber may clean hallways at night.
3.2.2 Disinfection
Disinfecting using U.S. Environmental Protection Agency (EPA)’s List N disinfectants kills any remaining germs on surfaces, which further reduces any risk of spreading infection. After manual processes, no-touch disinfection modalities also may be used, including ultraviolet (UV) light disinfection systems; hydrogen peroxide vapor, also referred to as vaporous hydrogen peroxide (VHP), steam; ozone; and chlorine dioxide vapor.[x]
UV light technology does not require changes in room ventilation, does not leave a residue, and has a broad spectrum.
UV light technology is a nonchemical approach to disinfection. UV light technology is also advantageous because it does not require changes in room ventilation, does not leave a residue after treatment, and has a broad spectrum of action. UV light has been successfully used to reduce the bioburden of a room enough to stop outbreaks associated with environmental contamination and FAIs transmitted from high-touch surfaces.[xi] UV light surface disinfection systems provide localized surface disinfection and spot treatment. These units should only be used to disinfect unoccupied spaces.
Several autonomous robotic technologies are available that use ultraviolet C (UV-C) lighting to disinfect and clean surfaces without staff assistance. UV-C is one of the classified subbands of ultraviolet light. These no-touch technologies use a high-intensity broad spectrum UV light that deactivates harmful germs. These fully automatic UV light machines disinfect high-traffic areas and shared spaces and can disinfect large areas of linear surface area during the night or when needed. Scheduling of disinfection can be initiated or modified from anywhere using a mobile device, browser, or integration with a scheduling system.
3.2.3 Methods for Evaluating Environment
There are several methods to evaluate the environment before or after cleaning and disinfection. Two examples include the following:
- Agar Slide Cultures: Agar-coated glass slides with finger holds were developed to simplify quantitative cultures of liquids. The slides have been adopted for use in environmental surface monitoring in health care settings. These studies have used agar-coated slide systems to quantify aerobic colony counts (ACCs) per cm and evaluate cleaning practice.While studies have measured aggregate ACCs before and after cleaning, no studies to date have evaluated how thoroughly the same objects were cleaned to determine if objects with relatively high ACCs were poorly cleaned or if staff overlooked cleaning them. Although some difficulties have been encountered in utilizing the agar slide cultures on surfaces other than large, flat surfaces, the cultures could provide an easy method for quantifying viable microbial surface contamination. To accurately assess cleaning practice, it is important to determine pre-cleaning levels of contamination for each object evaluated.
- Fluorescent Markers: Fluorescent gel, powder, and lotion have all been developed for the purpose of marking high-touch objects prior to room cleaning. While the powder and lotion have been used as part of educational interventions, their characteristics may limit their use in a monitoring system. Lotions and powder are overtly visible, powder can be disturbed with ease, and lotion that is allowed to air dry is difficult to remove. Little or no published experience with using these substances for this purpose is available.In contrast, the fluorescent gel dries transparent on surfaces and resists abrasion. Several studies demonstrate the system’s accuracy in objectively evaluating cleaning practice and quantifying the impact of educational interventions on cleaning.[xii] [xiii]These fluorescent markers are all designed to indicate physical removal of an applied substance and may be more effective. Using one of these markers rather than the culture techniques makes it more likely that surfaces that are effectively disinfected but less effectively cleaned will be flagged as failing to meet a quality standard.
For additional information, please visit Options for Evaluating Environmental Cleaning, from the CDC.
3.3 Air Filtration & Disinfection
According to the CDC, 69% – 90% of pathogens that cause infections are airborne. More than 90% of all infectious surface pathogens originate from the air. Therefore, it is critically important to focus more attention on air cleaning to stop pathogens before they land on surfaces or people inhale them.
HEPA filtration is not the best option, bipolar ionization is not recommended, and PCO air cleaners are less than ideal.
3.3.1 Minimum Efficiency Reporting Value (MERV) and High Efficiency Particulate Air (HEPA) Filtration
The most common methods of air purification within long-term care facilities are Minimum Efficiency Reporting Value (MERV) and High Efficiency Particulate Air (HEPA) filtration. HEPA filters have the highest efficiency and can be installed into the air handling unit (AHU) or into the ductwork that serves critical spaces.
They are mechanical filters that remove up to 99.97% of particulates that are 0.3 microns in size.[xiv] These particulates include dust, molds, biologicals, pollen, and other airborne particles. HEPA filters function by capturing the particulates and trapping them within the filter’s matrix. When the filter captures viable particulates, such as bacteria, fungus, and viruses, these pathogens can continue to grow within the filter. As they continue to grow and reproduce, the high velocity of the air passing through the filter can dislodge them, allowing them to reenter the airstream.[xv]
Once returned to the airstream, these harmful particulates can circulate within the spaces the filter was intended to protect. Because of this situation, HEPA filtration is not the best option for controlling pathogens and other viable particulates.
3.3.2 Bipolar Ionization
Another air purification technique that long-term care communities commonly use is bipolar ionization. Bipolar ionization devices generate positive and negative ions. The devices’ manufacturers claim that the ions generated attach to particulates in the air and cause them to agglomerate, forming larger particles that mechanical filters can remove more easily. The manufacturers also claim that the ions are capable of breaking down volatile organic compounds (VOCs) and that they can inactivate or kill airborne pathogens.
While bipolar ionization devices can decrease some hydrocarbons, they also increase other VOCs.
Studies have shown that though bipolar ionization devices can decrease some hydrocarbons, they also increase other VOCs such as acetone, ethanol, and toluene. Testing showed that ionizers had a minimal impact on concentrations of particulates, ozone, and nitrogen dioxide.[xvi] Additionally, little to no literature is available on the effectiveness of such devices on biologicals in real-world, live-operation environments. Use of bipolar ionization is not recommended, due to a lack of evidence surrounding its effectiveness and its potential to generate harmful byproducts.
3.3.3 Photocatalytic Oxidation (PCO) Technology
Photocatalytic oxidation (PCO) technology has been widely used for VOC remediation and to kill microbes. PCO devices operate by shining UV light onto a honeycomb-shaped reactor coated with a photocatalyst, most commonly titanium dioxide. The UV light interacts with the catalyst and generates hydroxyl radicals that can break down VOCs and kill microbes.[xvii] Though some PCO air cleaners can be effective in removing VOCs, they have also been shown to generate intermediate species and harmful byproducts.[xviii] The potential to generate harmful byproducts and incomplete oxidation makes this technology less than ideal for use in long-term care facilities.
AAPT provides the most comprehensive air purification available.
3.3.4 Advanced Air Purification Technology (AAPT)
A novel air purification technology exists that remediates all categories of airborne contaminants—VOCs, biologicals, and particulates. The advanced air purification technology (AAPT) is an in-duct system that is installed in the facility’s ductwork downstream of the air handler. The technology is comprised of five stages of air purification technology.
- The first two stages contain proprietary molecular media that is designed to remediate all VOCs to below detection.
- The third stage is a chamber that contains high dose UV-C and is modeled to mathematically and genomically kill all airborne pathogens and biologicals in a single pass through the system.
- The fourth stage contains a polishing VOC filter.
- The fifth stage is a HEPA filter to capture all particulates.
The AAPT provides the most comprehensive air purification available and has been tested in a 15-month Institutional Review Board (IRB) approved study in a long-term care facility. The study results showed an 88.43% reduction in airborne biological contaminants, a 96% reduction in infectious surface fomites, and an 89.88% reduction in VOCs. Additionally, the technology installation resulted in a 39.6% reduction in facility acquired infections (FAIs) and a 47% reduction in staff call-outs.
3.4 Health Screening
The health screening process includes components designed to identify and monitor suspected or confirmed infectious diseases. Ranging from temperature capture to symptom identification, health screening enables providers to not only manage confirmed infections, but also prevent individuals from exposing others to a suspected infection.
Technology’s purpose in health screening is to simplify the process of capturing health screening data, through use of a digital sign-in/kiosk system or other method of capture. A health screening questionnaire generally consists of generic demographic information, such as the individual’s name and contact information, that can be used later for trace tracking and notifications.
The process also captures additional information such as present symptoms, known exposure, and vaccination status. Depending on the facility’s policies as well as county, state, and federal guidelines or regulations, additional questions may be necessary. A good technology solution for health screening should also include an easy way to collect relevant documentation, such as proof of COVID or flu vaccination, TB clearance test results, etc.
Information captured throughout the screening process is then used to rule out possible exposure of an infectious disease to the facility’s population. If a suspected infection is identified, the facility is responsible for implementing infection control processes according to their policies.
A digital sign-in/kiosk system with back-end reporting tools can replace the cost of having staff handle screenings and reporting.
Another advantage of using technology to conduct health screening and contact tracing is cost reduction. A digital sign-in/kiosk system with back-end reporting tools can replace the cost of having staff manually sign in and/or take the temperature of every person entering a facility and give this manual sign-in information to other staff to enter into a reporting system. An individual entering a facility can “self-screen” at a kiosk by answering health screening questions, providing contact information, and getting their temperature automatically taken via an automated thermometer attached to the kiosk.
3.5 Contact Tracing
Contact tracing is used to identify and contact individuals who have been exposed to an infectious disease, in an effort to stop the chain of exposure. By leveraging sign-in and sign-out logs as well as health screening information, providers can trace back to individuals who may have been or are confirmed to have been exposed to an infectious disease.
After identification, the provider is responsible for contacting each individual, discussing the possible or known exposure event, explaining the symptoms to monitor for, and giving them precautions to implement to keep from exposing others.
3.6 Infection Surveillance, Control, and Reporting Software Solutions
Infection surveillance, control, and reporting software solutions are designed to help health care facilities track and control the spread of infectious diseases. These solutions typically include features such as the following:
- Surveillance: The ability to collect and track data on patients, staff, and visitors who have been diagnosed with an infectious disease or who have been in contact with someone who has been diagnosed.
- Control: The ability to use the data collected through surveillance to identify potential outbreaks and take steps to control their spread, such as implementing isolation protocols or contact tracing.
- Reporting: The ability to generate reports that can be shared with public health officials and other stakeholders, such as the CDC or WHO.
Overall, infection surveillance, control, and reporting software solutions can play an important role in helping health care facilities and public health officials respond to outbreaks of infectious diseases and prevent their spread.
4. Benefits of Infection Control Technologies
4.1 Reducing Infections among Staff and Residents
4.1.1 Ultraviolet C Devices
Much of the recent literature regarding UV-C robots discusses UV-C disinfection and SARS-CoV-2. In January 2022, Viana Martins et al. reviewed 60 recent studies and found that UV-C devices inactivated airborne SARS-CoV-2, an important finding in the current fight against the COVID-19 pandemic. UV-C disinfection remains an important part of preventing many other infections in health care settings.
More research about the efficacy of UV-C disinfection in special populations is warranted.
The seminal study, the Benefits of Enhanced Terminal Room (BETR) Disinfection Study—a large, randomized 2016 control trial—found that “patients admitted to rooms previously occupied by patients harboring a multidrug-resistant organism or C difficile were [10% to 30%] less likely to acquire the same organism if the room was terminally disinfected using an enhanced strategy.” The largest risk reduction occurred when a UV-C device was a part of the disinfection strategy.
This study demonstrated that UV-C light could be used as part of the standard of care for disinfection in rooms where discharged patients have multidrug-resistant organism infections or C difficile infections, leading to a change in many health care facilities’ disinfection practices.
In 2021, Rock et al. found that UV-C disinfection did not decrease vancomycin-resistant enterococcus or C difficile infections in immunocompromised patients.[xix] Although this result does not disprove the BETR study’s findings, Rock’s findings suggest that more research about the efficacy of UV-C disinfection in special populations is warranted.[xx]
Recent studies continue to affirm that electronic nudges improve patient safety.
4.1.2 Electronic Health Records (EHRs) / Electronic Medical Records (EMRs)
EMRs continue to become not only clinician documentation tools, but also data collection tools. As this shift occurs, it becomes increasingly important to harness the power of EMRs/EHRs to prevent FAIs. EMRs/EHRs are being used in this capacity in two innovative ways:
- As decision-support tools, helping guide clinicians to make decisions to prevent FAIs and
- As predictive modeling via machine learning, aiding clinicians and infection programs in targeting patients at greatest risk of developing an FAI.
Decision-support tools are electronic nudges or hard stops that either direct clinicians away from choosing an intervention that may increase the risk of an FAI or disallow a clinician to make that choice at all (typically with an override from a hospital epidemiologist or other hospital leader).
Recent studies continue to affirm that electronic nudges improve patient safety by decreasing inappropriate C difficile orders, increasing appropriate C difficile prescriptions, and decreasing inappropriate antibiotic prescribing. However, decision-support tools are most likely to be effective when they feel easy to use, useful for decision-making, and reliable.[xxi]
4.2 Increasing Quality of Care and Life
Infection control technologies that reduce facility-acquired infections and staff call-outs are paramount in improving the quality of care and quality of life for residents. Improvements in FAI rates have a direct positive impact on residents’ well-being and quality of life because residents are not getting sick as frequently.
These technologies can substantially improve the quality of care and quality of life for residents.
In addition, any patient with a respiratory issue will enjoy the benefits of clean, pathogen-free air. Cleaner air has also been linked to improved cognitive function and mental well-being. Reductions in staff call-outs limits the need for agency nurses to cover shifts. Maintaining familiar staff members improves residents’ quality of life, as residents can know the people who are caring for them. Residents’ stress is reduced when they are comfortable with their caregivers and their routine.
4.3 Reducing Operational and Health Care Costs
Using infection control technologies that reduce FAIs has a direct positive economic impact. The Centers for Medicare & Medicaid Services (CMS) provides fixed payments per resident per day to long-term care facilities. CMS withholds 2% of the total payment and allows the long-term care facilities the chance to earn back all or some of this payment based on performance. Health care performance is ranked based on hospital readmission rates. CMS also evaluates year-over-year quality of care improvements and ranks all U.S. facilities against each other.
Reducing FAIs will bring facilities considerable additional savings.
Facilities that employ infection control technologies that help to reduce FAI rates will realize year-over-year improvements along with an improved overall facility ranking. These improvements will help to maximize the facility’s CMS reimbursement.
Each facility-acquired infection may also require some or all of the following measures, which all cost money:
- Doctor Visits
- Isolation
- Increased Monitoring
- Licensed Nurse follow-up
- Medication
- Quarantines and Lockdowns
- Transfer to the Emergency Room: A resident who goes to the hospital may never return to the long-term care facility.
Therefore, reducing these infections bring facilities considerable additional savings.
Staff call-outs due to sickness require the long-term care facility to replace the staff member who has called out. This staff member can either be replaced by another employee or by an agency nurse. Replacement by another employee requires that the individual covering the shift come in when they were originally scheduled to be off or that their original shift be extended. In both instances, the long-term care facility will likely be required to pay overtime.
If the long-term care facility must hire an agency nurse, there is an additional economic burden, as agency nurses are traditionally more expensive than staff nurses. In addition, use of agency nurses is typically associated with increased care failures, such as falls and meal or medicine mix ups. A significant cost is associated with these care failures.
Any infection control technology that reduces airborne pathogens and infectious surface fomites can help reduce the frequency of staff call-outs and bring the facility a positive economic benefit.
4.4 Increasing Resident and Family Satisfaction
Reductions in facility-acquired infections have positive impacts on resident well-being and family satisfaction. When infection control technologies are implemented that reduce facility acquired infections, residents do not become sick as frequently and are not required to go to the hospital as often.
Remaining healthy and out of the hospital has significant benefits for resident and family happiness, well-being, and overall satisfaction. Family members are able to visit more frequently when staff and resident infections are lower, which benefits the resident and the family. It also improves the facility’s public reputation for new residents and families considering different care options.
4.5 Improving Public Health and Reporting Capabilities
Infection surveillance, control, and reporting software solutions can help improve public health and reporting capabilities in several ways:
- Early Detection: These systems can help health care facilities and public health officials quickly identify and respond to outbreaks of infectious diseases by collecting and analyzing data on patients, staff, and visitors who have been diagnosed with an infectious disease or who have been in contact with someone who has been diagnosed.
- Rapid Response: Once an outbreak is identified, these systems can help health care facilities and public health officials take steps to control its spread, such as implementing isolation protocols or contact tracing. These measures can help limit the number of people affected by the outbreak and reduce its overall impact on public health.
- Data Sharing: These systems can help public health officials share data with other stakeholders, such as the CDC or the WHO, which can help improve overall public health reporting capabilities.
- Data Visualization: Some systems provide data visualization tools that can help health care facilities and public health officials quickly identify patterns, trends, and hotspots related to infectious diseases, which can help inform decisions about how to respond to an outbreak.
- Automation: These systems can automate data collection, analysis, and reporting processes, which can help reduce errors and save time for health care facilities and public health officials.
Overall, infection surveillance, control, and reporting software solutions can play an important role in helping health care facilities and public health officials respond to outbreaks of infectious diseases and prevent their spread. These measures also help in reporting and tracking the data, which can be helpful in future outbreaks.
Staff call-outs bring negative economic and clinical impacts.
4.6 Reducing Staff Sick Leave
As described in Section 4.c., staff call-outs bring a negative economic impact. A negative clinical impact is also associated with staff call-outs, particularly when an agency nurse is brought in.
Many facilities are struggling with staffing shortages. As a result, these facilities cannot run at full capacity, as they do not have the staff to support additional residents or patients. This worker crisis further exacerbates the issues with staff sick leave, requiring the use of a much more expensive and potentially less effective agency nurse more frequently.
Reducing facility-acquired infections improves staff efficiency.
4.7 Increasing Staff Efficiencies
Reducing facility-acquired infections has a direct positive impact on staff efficiency. By not having to care for sick residents as frequently or fill out hospital transfer paperwork, the staff can focus solely on caring for the residents. In addition, when fewer staff members are out sick, there is greater continuity of care and workflow. The regular full-time staff is fully aware of routines and workflow patterns that make for greater efficiencies. When outside support is needed, it negatively affects these routines.
In addition to helping reduce avoidable exposure and outbreaks, an infection prevention and control solution should increase staff efficiencies. Some efficiencies, such as eliminating redundancy in workflows, create a return of labor hours. Other efficiencies, such as automating workflows and elevating regulatory compliance, create not only a return of labor hours but also a return of financial investment through avoidable civil monetary penalties.
Fewer infections lead to staff satisfaction and retention.
4.8 Increasing Staff Satisfaction and Retention
Infection-control technologies that reduce staff call-outs bring a direct positive impact on staff satisfaction and retention. Workers are happier when they are not required to frequently cover sick coworkers’ shifts. Further, staff members will have higher satisfaction working in an environment where they do not become ill often. The reduction in staff and resident infections will also help a facility attract new workers who will feel more comfortable in a safer environment.
4.9 Mitigating Risks and Liabilities and Improving the Community’s Reputation
To mitigate risks and liabilities, a provider should conduct routine process, quality, and competency audits. These activities are designed to not only uncover areas of risk, but also to ensure the provider has enough information to implement interventions to mitigate them.
Informed consents to staff, residents, and visitors can help to mitigate liability of exposure of infectious diseases. However, infection control processes should always be monitored and enforced, regardless of an individual’s acknowledgement.
Providers should also employ their Quality Assurance and Performance Improvement team to evaluate the facility’s infection control program. Detailed findings and plans to improve or eliminate risk should be documented thoroughly.
To ensure that improvement is ongoing, providers should identify measurable outcomes and methods to capture not only outcome data, but also data trends.
Certain activities directly affect the way residents, visitors, and staff perceive a provider.
These activities directly affect the perception a provider creates for their residents, visitors, and staff. Infection control has taken center stage because of the COVID-19 pandemic. As a result, providers should be hyper-focused on how their infection control program impacts their reputation.
5. Potential Long-term and Post-acute Care (LTPAC) Provider Business Models
5.1 Provider Relief Fund (CARES Act)
The Provider Relief Fund was established by the Coronavirus Aid, Relief, and Economic Security (CARES) Act and the Paycheck Protection Program and Health Care Enhancement Act. The $175 billion relief fund is designated to provide financial support to providers impacted by COVID-19 that experience either necessary expenses or declines in revenue attributable to the coronavirus. Of the $175 billion in relief funding thus far, $50 billion was set aside for health care providers and distributed in two tranches, or portions, as part of its general allocation distribution.
The Provider Relief Fund disbursements can be used to support expenses related to health care or lost revenue attributable to COVID-19 so long as the funds are used “to prevent, prepare for, and respond to coronavirus” and the terms and conditions applicable to the specific allocation are met.
NHIC payments may only be used to reimburse infection control expenses.
The Nursing Home Infection Control (NHIC) distribution is a component of a Provider Relief Fund (PRF) Targeted Distribution, formally known as the Skilled Nursing Facility and Nursing Home Infection Control Distribution. It is awarded to skilled nursing facilities and nursing homes nationwide to help combat the devastating effects of this pandemic. NHIC payments may only be used to reimburse infection control expenses. Nursing Home Infection Control payments may not be used to reimburse lost revenues. These payments may not reimburse expenses reimbursed by other sources or that other sources are obligated to reimburse.
Examples of allowable Nursing Home Infection Control expenses include the following:
- Costs of reporting COVID-19 test results to local, state, or federal governments.
- Retaining and hiring staff to provide patient care or administrative support.
- Expenses incurred to improve infection control, such as heating, ventilation, and air conditioning (HVAC) systems or sanitizing equipment.
- Expenses paid for information technology (IT) or interoperability systems to expand or preserve infection control during the reporting period, such as telehealth infrastructure, increased bandwidth, technology that permits residents to connect with their families, and teleworking to support remote workforce.
- Providing additional services to residents, such as technology that permits residents to connect with their families, if the families are unable to visit in person.
Ask these questions:
- Did this expense cover an infection control purpose?
- Was this expense to prepare for, prevent, or respond to coronavirus?
- Does it comply with the Terms and Conditions?
- Do we have documentation to support this claim?
For more information, please check out the Health Resources & Services Administration website and Technical Assistance Session slide deck.
5.2 Commercial Property-Assessed Clean Energy (C-PACE)
C-PACE is an innovative funding tool that allows long-term care facilities to preserve their capital expenditure (CapEx) budget and still maximize the benefits of building upgrades that make their property more valuable. It is not a loan and therefore does not affect one’s credit score or ability to take out a traditional loan. Here is how it works.
- C-PACE allows for building upgrades to be completed with $0 out-of-pocket and positive cash flow that can be achieved in the first year. Projects can include building envelope, renewable energy, resiliency, wellness, and efficiency upgrades.
- C-PACE can be on or off balance sheet and is funded by private investors and government programs. It is a long-term (typically 20 years), low-risk funding program.
- The project’s energy savings and incentives must exceed the cost of the project, or it will not be funded. Therefore, C-PACE projects increase an organization’s bottom line.
- A third-party, certified, licensed professional must approve that the project’s energy savings exceed the costs, or it will not be approved.
- To complete a C-PACE project, building owners can contact their local C-PACE program to connect with lenders and contractors, or they can reach out to an energy master planner to help manage the project.
- C-PACE acts as a property tax and is transferred to the new building owner if the building is sold.
- C-PACE is the solution to optimizing a building and increasing its value in a way that makes good business sense. It is the solution to deferred maintenance; Environmental, Social, and Governance (ESG) ratings; upcoming emissions penalties; and more.
Eligibility highlights are as follows:
- Currently available in 32 states and Washington, DC.
- New and existing commercial and long-term care buildings, including nonprofits.
See PACENation for the latest market data.
5.3 Civil Money Penalty Funds (CMP)
Up to $3,000 in grant funding may be available for indoor air quality improvements on a state-by-state basis for certified nursing facilities through the Civil Money Penalty Reinvestment Program.
5.4 Potential Affordable Care Act (ACA) Opportunities
The Affordable Care Act (ACA) is shifting the health care system in the United States away from the traditional fee-for-service to a pay-for-performance system. This change is starting to eliminate the misalignment of incentives inherent in traditional Medicare, Medicaid, and private insurance programs.
There are many provisions and models in the ACA that would benefit from, provide opportunities to cover, and consequently encourage the adoption of infection control technologies.
New Models
The ACA created the Center for Medicare & Medicaid Innovation (CMMI), which is tasked with exploring new care delivery and payment models and initiatives that do the following:
- Use more holistic, patient-centered, and team-based approaches to chronic disease management and transitional care.
- Improve communication and care coordination between and among care providers.
- Improve care quality and population health while reducing growth in expenditures.[xxii]
The ACA puts explicit emphasis on the use of health IT, including safety and remote patient monitoring, in Health Homes for Enrollees with Chronic Conditions, the Independence at Home Demonstration, and the Use of Technology in New State Options for Long-Term Services and Supports. These initiatives include the following:
- Hospital Readmission Reduction Program (HRRP).[xxiii]
- Accountable Care Organizations (ACOs).[xxiv]
- Bundling of Payments models; the following are relevant to LTPAC providers:
New care delivery and payment models may enable LTPAC providers using technologies to derive revenues from strategic partners.
LTPAC providers bring a significant value for hospitals, physician groups, payers, and accountable care organization (ACO) partners by providing the following services:
- Rehabilitation and skilled nursing facilities that provide post-discharge/post-acute patient rehabilitation.
- Skilled nursing facilities, assisted living facilities, continuing care retirement communities, housing with services, and home health agencies that provide post-acute patient stabilization and sub-acute chronic disease management.
- Holistic person-centered care, including support services.
- Lower-cost care settings than hospitals.
These new care delivery and payment models will give LTPAC providers using technologies—like health IT, safety, and remote patient monitoring technologies—opportunities to derive revenues from strategic partners.
Private insurance companies may cover the cost of infection control technology.
5.5 Private Insurance
Private insurance companies may cover the cost of infection control technology, depending on the specific policy and the technology in question. It is best to check with the insurance company directly to determine coverage.
5.6 Private Pay
Other payment sources for infection control technologies and services may be private payers or out-of-pocket payments by residents or clients.
5.7 Standard of Care
LTPAC and community health providers, special population agencies, self-pay and self-insured organizations, and others, especially nonprofits, may offer an array of infection control technologies and services. Grants may cover these services. Or the organization may absorb the cost, with different revenue sources covering it, including charitable contributions.
5.8 Return on Investment (ROI) of Infection Control Technologies
ROI represents the ratio of the net gains relative to the initial investment over a certain period of time. Subsequently, ROI can be expressed in the following equation:
![]()
As discussed above, infection control technologies deliver various benefits, including potential financial savings, to different stakeholders. Stakeholders include patients and/or their families, payers, care providers, etc.
However, the financial savings and ROI depend on a number of factors, including the care/service delivery model, the payment/reimbursement model, the technology, and of course costs. The first and most important step in calculating ROI is to consider the different stakeholders, identify the investors, and calculate the gains and savings netted/accrued to each investing stakeholder under each particular care delivery and payment model.
Often the reduction of hospital days is erroneously included in the provider’s ROI.
When calculating ROI, one should only include the gains that accrued to that particular stakeholder minus all expenses, relative to that stakeholder’s own investment/cost. Often the reduction of hospital days is erroneously included in the provider’s ROI, which is not true under the traditional fee-for-service reimbursement model and can be misleading; such a reduction usually accrues to the payer.
5.8.1 ROI to Patients and/or their Families
ROI to patients and/or their families can be calculated as follows:
![]()
For private pay patients and their families, for example, the financial gains of infection control technologies are in prolonging independence by delaying the transition to a higher and more-costly level of care. These benefits are significant.
The gains may also include savings in co-pays for recurring hospital visits, and of course peace of mind for the individual and their family, which is difficult to quantify. The patient’s and family’s expenses are the monthly out-of-pocket cost of safety technologies, plus any co-pay for the occasional interventions.
5.8.2 ROI to Payers
ROI to payers can be calculated as follows:
![]()
For dual Medicare and Medicaid eligible patients who are nursing home eligible, for example, the financial gains of infection control technologies under a Medicaid Managed Care program that accrue to program depend on keeping patients in their own homes with home health, home care, and other supportive services. Otherwise, the managed care would be liable for the costs of nursing home room and board.
Managed care’s investment is the monthly rate of infection control technology, as well as home- and community-based supportive services aimed at keeping the individual independent.
Additional savings, like reductions in hospitalization and hospital readmission costs, may accrue to Medicare or the managed care plan. Consequently, such savings or gains should be correctly attributed.
The care provider investing in infection control may gain lower infection rates and higher payments as incentives.
5.8.3 ROI to Care Provider
ROI to care providers can be calculated as follows:
![]()
The care provider who makes investments in infection control technology infrastructure may gain these benefits:
- Lower rate of infections in both residents and staff.
- Higher reimbursements/payment from the payer or strategic partner as incentives for avoiding more costly care settings, procedures, events, or penalties.
For example, an LTPAC provider partnering with a physician group ACO to manage a chronically ill patient population can potentially get a percentage of the incentives or shared savings payments the ACO receives from the payer for reducing hospitalizations and hospital readmissions. These amounts can be significant for certain populations.
5.8.4 LTPAC Provider
The LTPAC provider’s net gain is the same as above
+ Plus the sum of all gains accruing to the LTPAC provider in staff efficiencies, increased referrals from the ACO, increased traditional fee-for-service rates, and additional incentive payments received from the ACO.
– Minus the costs of leasing the safety monitoring equipment and actual costs of services delivered.
5.8.5 Physician Group ACO
The physician group ACO’s ROI is the same as above
+ Plus the portion of the payer’s incentive payment that it gets to keep plus any additional fee-for-service payments due to more frequent office-based services
– Minus the actual costs of services it delivers (for example in medication reconciliation or care coordination), relative to the portion of incentives it passes through to the LTPAC provider.
In contrast, in a partnership between an LTPAC provider and hospital under the traditional fee-for-service model, for example, the LTPAC provider may help its hospital partners reduce falls and consequently all-cause 30-day readmission rates. This scenario helps the hospital avoid Medicare’s payment penalties under the Hospital Readmissions Reduction Program.
The hospital may contract with and pay the LTPAC provider a percentage of the penalties saved for delivering safety monitoring and fall prevention programs that lead to reducing 30-day readmissions for patients discharged from the hospital after being admitted for one of these three conditions.
5.8.6 Hospital
The hospital’s ROI is the same as above
+ Plus the portion of avoided penalties it gets to keep, plus any additional fee-for-service payments it gains for more referrals and increased rates due to improved quality ratings.
– Minus the actual costs of services it delivers, relative to the portion of avoided penalties it passed through to the LTPAC provider.
+ Plus any additional costs incurred for staff time in infection control and/or supportive services, for example.
6 Planning for and Selecting Appropriate infection Control Technology
6.1 Understanding the Population, Issues, Care Settings, Needs, Program Services, and Partners
Infection control technologies are important, but how effective is a technology if staff or residents are resistant to using the technology? Planning and selecting the technology that best fits each environment’s needs is crucial. Furthermore, the infection control technology should supplement an organization’s overall infection control program and infrastructure. This CDC assessment tool may be helpful.
Being proactive in assessing the needs of residents, staff, and family members is critical to choosing infection control technology.
Being proactive in assessing and even anticipating the needs of residents, staff, and family members is critical to planning, selecting, and supporting the most appropriate infection control technology for each unique setting.
The planning and selection process should include understanding the population the organization serves, be it independent, assisted, skilled care, memory care, rehabilitation, hospice, or a combination of all of the above. The organization’s constituencies drive the issues and needs that the level of care and programs must address. Infection control technologies are not one size fits all; thoroughly understanding and assessing the organization is recommended before selecting a partner or partners.
6.2 Planning for and Selecting Appropriate Infection Control Technology
6.2.1 Visioning and Strategic Planning
Visioning and strategic planning are necessary to make senior living communities successful and sustainable. The incorporation of technology, once a result of strategic planning, has now become its catalyst. Emerging technologies such as robotic disinfection and health screening systems play a critical role in community infection control, which incoming residents expect. Regulatory requirements or environmental factors may affect the time to incorporate infection control technologies. However, to begin planning for infection control technology, stakeholders must make a strong commitment to provide a safe living environment.
The success of an infection control technology solution requires the operator to identify the facilities’ or organization’s needs. These may include reducing technology stacks, elevating compliance and safety, improving avoidable outbreak rates, relieving staff from manual paper processes, and so on.
Once needs are identified, providers should focus on prioritizing needs based on their impact to operations, clinical outcomes, workforce, and fiscal health. What needs are requirements vs. “nice to have”? Which needs does everyone agree on as requirements to select an infection control technology?
6.2.2 Organizational Readiness Assessment
Consider several areas when assessing an organization’s readiness for certain infection control technologies.
6.2.2.1.1.1 Physical and IT Infrastructure
Convergence refers to the confluence of voice, data, wireless, and even body-area networks that provides an unprecedented level of connectivity. The beauty of the World Wide Web is the world-wide part. Wi-Fi in buildings and cellular outside of buildings allow roaming and handoff from office to home and anywhere in between.
The meshing of networks and devices has created the Internet of Things, with Cisco’s Internet Business Solutions Group predicting some 25 billion devices were connected in 2015, and 50 billion by 2020.
The power of this persistent connection makes it possible to do all sorts of great things. As a result, organizations can leverage data networks—not just rely on them. By assessing the current infrastructure, organizations can plan to augment it with technology they select.
It is important to learn about technologies’ function, uses and benefits, high-level network requirements, and connectivity requirements.
6.2.2.2 Available Technology Solutions
It is important to learn about the types of infection control technologies available, how they function, their uses and benefits, their high-level network requirements, and the connectivity they require.
As discussed above, the main categories of solutions include the following:
- Hand Hygiene Compliance
- Surface/Object Cleaning and Disinfection
- Air Filtration and Disinfection
- Health Screening
- Contract Tracing
- Infection Surveillance, Control, and Reporting Software Solutions
Because infection control technology spans such a broad range of technologies and unique categories, it is very likely for an organization to have multiple partners. With the ideal infection control systems in mind, consider the type(s) of infection control solutions needed and these questions:
- Does the system allow for customizable health screening questions?
- Can the system components be easily replaced, such as UV-C germicidal lamps?
- Does the technology integrate, interface, or interoperate with existing technologies?
- How long does it take to clean or disinfect a standard size room?
What types of reminders are used?
6.2.2.3 Available Data
Infection control technology can assist both staff members and residents, and data related to all stakeholders is important. This data can reside in human resources systems, visitor management systems, point of service systems, infection control software systems, security systems, and a variety of other databases. Assessing this data is important to avoid having redundant systems or competing databases of information when introducing new systems into any environment.
6.2.2.4 Additional Data Needed and Sources
Consider other sources of data that the residents may be bringing that may help an organization achieve its goals. Personal monitoring and tracking devices, like activity trackers, may be an example of such data sources.
Choosing the right technology for the current and future environment will create operational efficiency, interoperability, and cost savings.
6.2.2.5 Interoperability/ Interfacing Capability
Although isolated technologies are often powerful, they are amplified when combined and harnessed in a technological ecosystem. Interoperability allows the community to have a strategic comprehensive and holistic system of emergency alerting and response management, rather than multiple disjointed systems and response plans. Inefficient, standalone alarms can become detailed alerts with the right integration strategy.
Making the right technology decision that works in the existing and future environment will help create operational efficiency and interoperability that will enable cost savings. Maximize the return on technology investments by converging technology silos in the ecosystem where information is streamlined and caregivers can focus on providing care, including the social component of care. Technology integration empowers older adults to live safe, secure, connected, and purposeful lives.
6.2.2.6 Staff Needs
Staff needs often depend on the populations and care settings of those they are serving. Take into account the importance of mobility, on-site versus off-site notification, accountability requirements, proactive versus reactive care, and the organization’s brand promise.
6.2.2.7 Staff Competencies and Availability
The staff’s technical aptitude should be a factor in selecting infection control technologies for a community, but not a driving one. Ease of use should be considered regardless of the staff’s skill level. No technology should compete for the time staff should be dedicating to residents. Ongoing training should always be a part of the overall plan to support any technology, but especially one that impacts life safety and security.
Selecting a technology partner dedicated to innovation is the first step.
6.2.2.8 Partner Assessment
Selecting a technology partner dedicated to innovation is the first step. There are a lot of technology “vendors.” Choose a partner instead. Good partnership requires deep resources to create a positive experience for all aspects of an organization. Selecting a partner who is dedicated to innovation and a convergence strategy, and who can assist in evaluating workflow and processes, is important to overall success.
According to a provider in the technology field addressing the future of senior living, “While investing in new and advanced forms of technology for senior living facilities can be expensive and time consuming, it is critical to staying relevant in the industry and meeting the growing demand of residents. As communities look at new projects or go through refinancing on existing communities, it is important to engage technology experts and include forward-thinking solutions in the budget planning process.”
Careful assessments lead to a successful project.
6.2.2.9 Considerations for Resident/ Client and Family-Facing Solutions
Carefully assessing needs, competencies, personal preferences, and provider services and responsibilities leads to a successful project.
- Assess Issues/Needs, Including Special Needs: It is important to consider resident/client needs and preferences when selecting an infection control technology. This includes any special needs, like hearing or vision impairments, as well as preferences that increase likelihood of acceptance and adherence with use.
- Assess Competencies/Abilities: Assessing issues and special needs is usually the first part of the care planning process and of selecting a specific infection control technology solution that the resident/client will use. Furthermore, if the resident/client has a special need, like hearing or visual impairment, those needs must be considered when selecting the appropriate infection control solution and health screening modality.
- Assess Personal Preferences: Personal preferences may be important factors in whether the residents/clients use or are satisfied with the technology. For example, an air filtration system may produce a noise that is unsatisfactory to the resident. Another example may include a resident that may not want to use a touchscreen health screening kiosk. However, that resident may use a touchless option to interface with the kiosk.
- Assess Provider Services and Responsibilities: Care providers will need to review with the patient and family the common challenges and pitfalls that can hinder the proper development and implementation of infection control technologies. In addition, providers will need to identify the appropriate person or persons to maintain the infection control plan and communicate the patient’s needs if those needs are not being met.
Consider the implications of the type of solution on the existing IT infrastructure.
6.2.2.10 Physical and IT Infrastructure
Consider the implications of the type of solution on the existing IT infrastructure, including network, internet access, speed, and bandwidth. Remember that project implementation begins with updating IT infrastructure.
The technical team should have a few stakeholders as part of the implementation team. The technology vendor could provide plenty of implementation and troubleshooting support. Internally, the implementation team should be comprised of a technology lead (decision-maker in IT) and an implementation coordinator who is able to manage the relationship with the technology vendor and play a vital role in the initial implementation measures at the very least. Additional support technicians might be needed internally, but this step comes at a considerable cost if not kept small.
It is a good idea to engage the IT team members early in the process. They may have ideas, be familiar with new solutions, and be more enthusiastic when they are involved.
6.2.2.11 Operating Environment
The operating environment includes the care setting, the state in which the community is located, and the applicable federal and state regulations.
6.2.2.12 Operational and Programming Planning
Project Team: Operations team members will play a key role in implementation success, as they are the most connected to the people they serve. Ensure that operational leaders have buy-in early, and work alongside of them to identify the best individuals in the field to become evangelists. The key to engaging field operations in the initiative’s goals—such as nurses, therapists, certified nursing assistants, activity directors, and administrative staff—is that they are not salespeople; they are the connection evangelists.
The technology’s goals should be evaluated continuously and updated as programs change.
Goal Setting: Defining the infection control technology goals is critical to measuring success. Each organization will have different ideas of what success looks like based on strategic goals and internal operations. Before starting an infection control program, the organization should set a clear series of goals and metrics.
Keep in mind that goals should be measurable and routinely reported on within the organization’s operations. Ensure that they are SMART goals:
- Specific.
- Measurable.
- Attainable.
- Realistic.
- Trackable.
Setting both short-term and long-term goals for the infection control technology program is highly recommended. The program will naturally change and progress over time. Organizational goals set at the program’s start will likely be different six to 12 months post-implementation. The goals should be evaluated continuously and updated as programs change. It is also important to understand that a new program will have the ability to achieve several major goals during its initial adoption.
Program Design: Infection control technology programs should be designed with the organization’s short- and long-term goals in mind to help ensure success. Each program’s design should always consider how to align objectives, strategies, and technical plans by using infection control technology. Be sure to share experiences from other similar organizations to assist in strategies to build a safety technology program within the organization or strengthen an existing one.
Before starting any program, clearly define the new model of care and prepare staff with training and support plans.
When choosing technology, consider the setting, vendor support, legal requirements, hardware and software needs, and more.
6.2.2.13 Technology Review and Selection
When choosing technology, be sure to consider a wide range of factors, from the setting to vendor support, legal requirements, hardware and software requirements, and more.
Setting: The planning process would help identify key requirements that should include the care setting(s) where the organization wants to deploy the infection control solution; this should be the primary setting for the target population (home health, skilled nursing facility, housing with services, etc.).
Infection Control Modality: The planning team should also consider the system modality types, which include one or more of the following:
- Hand Hygiene Compliance
- Surface/Object Cleaning and Disinfection
- Air Filtration and Disinfection
- Health Screen
- Contract Tracing
- Infection Surveillance/Control/Reporting Software Solutions
System Embodiment: The planning team should consider the desired system embodiment, which may include the following:
- Monitored Dispenser
- Pendant
- Wristwatch/Smartwatch
- Badge
- Radio-frequency identification (RFID) Tagged Clothing
- Smartphone/Tablet
- Key Card/Fob
- Desktop
- Kiosk
- Passive Sensors
- Video
- Robot
- Cleaning/Disinfection Chamber
- Human-Operated Cleaning/Disinfection Machine
- Lighting System/Ceiling Fan
- Portable Units (Air Filtration/Disinfection)
- In-Duct Units (Air Filtration/Disinfection)
- Wall-Mounted Units (Air Filtration/Disinfection)
- Custom Solutions (Integrate with HVAC/Air-handling System)
Program Development and Vendor Support: The available resources, capabilities, and expertise in program design and operationalization would inform the type and level of development and support needed from the prospective vendor. These may include the following:
- Program Development (Planning, Design, Business Model Templates, Workflows, Change Management, etc.)
- Staff Training
- Caregiver Training
- User Education
- User Training
- User Engagement (such as Strategies for Sustained Usage)
- Family Engagement
Program Support Services: The support services that vendors may offer include the following:
- Equipment Delivery/Pickup
- Site/Home Installation
- IT/Network Troubleshooting and Support
- Front-End System Setup/Customization
- Back-End System Setup/Customization
- On-site/Online Staff Training
- On-site/Online User/Patient Training
- Equipment Cleaning/Refurbishing
Legal and Regulatory Requirements: Of course, legal requirements are important. Please consider the following requirements:
- Health Insurance Portability and Accountability Act of 1996 (HIPAA) (if applicable)
- Health Information Technology for Economic and Clinical Health (HITECH) (if applicable)
Hardware and Software Requirements: Finally, hardware/software requirements that could guide the selection process include how software is offered:
- Local Model: The software needs to be installed on servers local to the care provider.
- Third-Party Hosted Model/Software as a Service Model (SaaS): The software is hosted somewhere else, and the provider pays licensing and hosting fees or pays for usage, as opposed to maintaining local servers’ infrastructure.
Other important hardware and software requirements include remote access functionality support, offline functionality support when running third-party hosted or SaaS software, and mobile device support, such as for smartphones and tablets.
LeadingAge CAST resources help providers learn about available technologies and narrow their list.
Narrowing the List of Possible Solutions: LeadingAge CAST has several resources to help providers learn about infection control technologies on the market and narrow their list.
- Use the CAST Infection Control Online Selection Tool to narrow down the selection to a few shortlisted candidate systems and vendors that meet the must-have high-level requirements.
- In the CAST Infection Control Technology Selection Matrix, CAST outlines many additional options and detailed features and functionalities. These details will help drill down into these shortlisted products and narrow the selection to a list of two or three vendors who can be invited to submit a response to a request for proposals (RFP).
- During the RFP process, providers are encouraged to interview prospective vendors and engage many staff in the interviews and product evaluation: front staff, nursing and medical directors, care managers/ coordinators, and representatives from management, finance, and IT teams.
- Please check provider case studies with the vendors, including case studies collected by CAST, and conduct appropriate due diligence, including reference checking. In addition, providers may want to use the LeadingAge Member Community to ask peers about the shortlisted products and their experience with these vendors.
6.2.2.14 Implementation
The implementation and planning phase takes the information gained by the assessment phase and begins to answer the “who,” “how,” and “when” questions. During this phase, executive steering committee members are identified, and a project charter is created. Enough time should be set aside for this phase, as it is involved and detailed.
Contingency planning is part of the overall plan; the team must assess and identify potential risks throughout the project and deal with them quickly. Most often, risk is not going to severely impact the project. However, when a risk that could impact the project’s timeline, budget, or goals appears, the steering committee should be made aware to make decisions.
6.2.2.15 Post-Implementation Monitoring
It is important to provide continuous monitoring of any program. Monitoring validates the program, tracks improvement, and identifies any new problems that may occur. Measuring the program’s quality will provide an opportunity to establish its positive impact on the organization, consumers, and any partners. If post-monitoring does not show significant differences in care planning and coordination for those individuals served, the organization will need to rethink the program.
7. Acknowledgement of Contributors
7.1 Contributing Writers
Dave Becattini, LifeAire
Lever Stewart, Accushield
TK King, Accushield
Scott Code, LeadingAge
7.2 Workgroup Members
Dave Becattini, LifeAire
Jim McGovern, Christ’s Home Retirement Community
Joel Snyder, Friendly Senior Living
Judy Collett-Miller, Parker Life
Lever Stewart, Accushield
Majd Alwan, formerly LeadingAge
Ryan Elza, Volunteers of America National Services
Scott Code, LeadingAge
8. References
Price DL, Simmons RB, Crow SA, Ahearn DG. Mold colonization during use of preservative-treated and untreated air filters, including HEPA filters from hospitals and commercial locations over an 8-year period (1996-2003). J Ind Microbiol Biotechnol. 2005 Apr 26;32:319-321.
United States Environmental Protection Agency. What is a HEPA filter? [Internet]. [place unknown]: United States government; 2022 [updated 2022 Apr 26; cited 2022 May 25]. Available from: https://www.epa.gov/indoor-air-quality-iaq/what-hepa-filter.
Zeng, Y.; Manwatkar, P.; Laguerre, A.; Beke, M.; Kang, I.; Ali, A.; Farmer, D.; Gall, E.; Heidarinejad, M.; Stephens, B. Evaluating a Commercially Available In-Duct Bipolar Ionization Device for Pollutant Removal and Potential Byproduct Formation. Build. Environ. 2021, 195, 107750, DOI: 10.1016/j.buildenv.2021.107750
Hodgson AT, Destaillats H, Sullivan DP, Fisk WJ. Performance of ultraviolet photocatalytic oxidation for indoor air cleaning applications. Indoor Air. 2007;17:305-316.
Wargocki P, Kuehn TH, Burroughs HEB, Muller CO, Conrad EA, Saputa DA, Fisk WJ, Siegel JA, Jackson MC, Veeck A and Francisco P. ASHRAE position document on filtration and air cleaning, www.ashrae.org (2015, accessed 5 October 2022).
9. Resources
- https://www.ncbi.nlm.nih.gov/books/NBK519017/
- https://www.cdc.gov/infectioncontrol/basics/index.html
- https://www.ahrq.gov/hai/quality/tools/cauti-ltc/modules/resources/guides/infection-prevent.html#:~:text=Infection%20prevention%20and%20control%20practices,from%20getting%20infections%20from%20residents .
- https://www.infectioncontroltoday.com/view/ltc-facilities-face-unique-infection-control-issues-during-covid-19-pandemic
- https://www.cdc.gov/handwashing/index.html
- https://www.cdc.gov/clean-hands/data-research/facts-stats/?CDC_AAref_Val=https://www.cdc.gov/handwashing/why-handwashing.html
- https://www.researchgate.net/profile/John-Boyce-3/publication/51655480_Measuring_Healthcare_Worker_Hand_Hygiene_Activity_Current_Practices_and_Emerging_Technologies/links/541b34ff0cf2218008c05848/Measuring-Healthcare-Worker-Hand-Hygiene-Activity-Current-Practices-and-Emerging-Technologies.pdf
- https://researchforevidence.fhi360.org/sensing-technology-a-superior-alternative-for-improving-hand-hygiene-compliance-in-health-care-settings
- https://www.cdc.gov/infectioncontrol/guidelines/disinfection/cleaning.html
- https://www.ncbi.nlm.nih.gov/books/NBK563017/#:~:text=After%20manual%20processes%2C%20no%2Dtouch,ozone%2C%20and%20chlorine%20dioxide%20vapor.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8869636/
- Carling PC, Parry MM, Rupp ME, Po JL, Dick BL, Von Beheren S. for the Healthcare Environmental Hygiene Study Group. Improving cleaning of the environment surrounding patients in 36 acute care hospitals. Inf Control Hosp Epidem 2008; 29:11,1035-1041.
- Goodman ER, Platt R, Bass R, Onderdonk AB, Yokoe DS, Huang SS. Impact of an environmental cleaning intervention on the presence of methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci on surfaces in intensive care unit rooms. Infect Control Hosp Epi Demiol 2008; 29:593-599.
- [1] Price 2005.
- [1] United States Environmental Protection Agency 2022.
- [1] Zeng 2021.
- [1] Hodgson 2007.
- [1] Wargocki 2015.
- [1] Anderson DJ, Chen LF, Weber DJ, Moehring RW, Lewis SS, Triplett PF, Blocker M, Becherer P, Schwab JC, Knelson LP, Lokhnygina Y, Rutala WA, Kanamori H, Gergen MF, Sexton DJ; CDC Prevention Epicenters Program. Enhanced terminal room disinfection and acquisition and infection caused by multidrug-resistant organisms and Clostridium difficile (the Benefits of Enhanced Terminal Room Disinfection study): a cluster-randomised, multicentre, crossover study. Lancet. 2017 Feb 25;389(10071):805-814. doi: 10.1016/S0140-6736(16)31588-4. Epub 2017 Jan 17.
- [1] https://www.infectioncontroltoday.com/view/latest-advancements-in-infection-prevention-technology
- [1] https://www.infectioncontroltoday.com/view/latest-advancements-in-infection-prevention-technology
- [1] CMMI Innovations Models and Initiatives, CMMI, CMS. Available online at: https://innovation.cms.gov/initiatives/index.html.
- [1] Medicare Hospital Readmission Reduction Program, CMS. Available online at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html.
- [1] CMS ACO Initiatives, CMMI, CMS. Available online at: https://innovation.cms.gov/initiatives/ACO/.
- [1] Retrospective Acute Hospital Stay plus Post-Acute Services Payment Bundling Demonstration, CMMI, CMS. Available online at: https://innovation.cms.gov/initiatives/BPCI-Model-2/.
- [1] Retrospective Post-Acute Care Only Payment Bundling Demonstration, CMMI, CMS. Available online at: https://innovation.cms.gov/initiatives/BPCI-Model-3/.