The COVID-19 public health emergency (PHE) is still in place until January 11, 2023 (it was renewed for 90 days on October 13, 2022). We should know imminently whether the PHE will be renewed in January; HHS has promised states 60 days’ notice prior to the end of the PHE and that 60-day mark is on Saturday Nov 12th and given that Friday Nov 11th is a Federal holiday, we’ll be watching on Thursday Nov 10th!
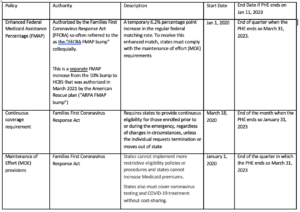
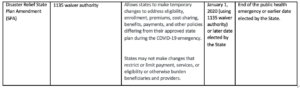
First, here are the policies that are in place currently related to the PHE[1]:
[1]Adapted from https://www.kff.org/report-section/medicaid-maintenance-of-eligibility-moe-requirements-issues-to-watch-appendix/
The continuous coverage provision means that states have been unable to disenroll anyone from the Medicaid program since the beginning of the pandemic. So even if a state continued renewals during the pandemic, they have not been permitted to terminate coverage. Therefore, an “unwinding” will occur, but the extent of the unwinding will vary from state to state. Once the PHE ends, states will have 12 months to initiate redeterminations of Medicaid and CHIP eligibility for all enrollees and two additional months (14 months total) to complete all the administrative work associated with these redeterminations.
Included in the resources today is a link to CMS’ extensive landing page with unwinding resources. In particular, go to the FAQs from October which has a lot of great information on unwinding. CMS has been putting out information on unwinding since the spring and has offered states a lot of technical assistance and opportunities for waivers to ensure the unwinding goes as smoothly as possible. However, we still anticipate a rocky road. So what should you do?
- Talk with your state LeadingAge partner to see what they are hearing about the unwinding plan in your state and what you need to be ready for;
- Make sure your relevant residents and clients know that they will likely have to undergo a Medicaid redetermination in 2023. You can tell them to be on the lookout for mail from the State and not to throw it away. An ASPE report that looked at the potential for churn in the Medicaid program due to the end of PHE policy predicted that 21% of eligible older adults (65+) may lose their coverage for a period of time due to administrative churn – let’s defy expectations on that one![1]; and
- Be prepared that you may have clients or residents who might no longer be eligible for Medicaid and have an organizational plan about how to address this.
LeadingAge will organize education on the unwinding and its impacts once the end of the PHE is officially announced but please feel free to reach out to Mollie at mgurian@leadingage.org with any questions in the meantime.
[1]https://aspe.hhs.gov/sites/default/files/documents/60f0ac74ee06eb578d30b0f39ac94323/aspe-end-mcaid-continuous-coverage.pdf

 Shutdown Week Three: Impact of Ongoing Closure on Affordable Housing
Shutdown Week Three: Impact of Ongoing Closure on Affordable Housing Colleagues on the Move, February 18, 2026
Colleagues on the Move, February 18, 2026