Functional Assessment and Activity Monitoring Technology: A Primer and Provider Selection Guide
Home » Functional Assessment and Activity Monitoring Technology: A Primer and Provider Selection Guide
Home » Functional Assessment and Activity Monitoring Technology: A Primer and Provider Selection Guide
1 Purpose of White Paper
1.1 Purpose
1.2 Disclaimers
2 Functional Decline
2.1 Definition
2.1.1 Connection to Chronic Conditions, Cognitive Decline, and Lifestyle
2.2 Prevalence
2.3 Cost and Burdens Associated
3 Definition/Types of Functional Assessment and Activity Monitoring Technologies (Non-Mutually Exclusive Categories):
3.1 Definition
3.2 Types of Functional Assessment
3.3 Activity Monitoring Technologies
3.3.1 Passive Monitoring Systems
3.3.2 Active Monitoring Systems
4 Potential Uses and Benefits of Functional Assessment and Activity Monitoring Technologies
4.1 Overview
4.2 Activities of Daily Living (ADL) Monitoring
4.3 Instrumental Activities of Daily Living (IADL) Monitoring
4.4 Functional Assessment
4.5 Physical Activity and Other Parameters
4.6 Uses for the Information
5 Benefits of Functional Assessment and Activity Monitoring Technologies
5.1 Active Lifestyle and Behavior Change
5.2 Weight Loss and Combating Obesity
5.3 Improving Gait and Reducing Fall Risk
5.4 Family Caregiver Engagement to Prevent Costly Transitions
5.5 Health Care Costs
6 Potential Long-Term and Post-Acute Care (LTPAC) Provider Business Models
6.1 Medicare, Medicaid, and Private Health Insurance Coverage
6.1.1 Program of All-Inclusive Care for the Elderly (PACE)
6.2 Medicaid Waiver Coverage
6.3 Potential Affordable Care Act (ACA) Opportunities
6.4 Private Pay
6.5 Standard of Care and Other Payment Sources
6.6 Return on Investment (ROI) of Telehealth and RPM
6.6.1 ROI to Patients and/or Their Families
6.6.2 ROI to Payers
6.6.3 ROI to Care Provider
6.6.4 Online ROI Calculator
7 Planning for and Selecting Appropriate Functional Assessment and Activity Monitoring Technology
7.1 Understanding the Setting, Population, and Issues
7.1.1 Gemba Rounds
7.1.2 Systems Thinking
7.2 Planning for Functional Assessment and Activity Monitoring Solutions
7.2.1 Visioning and Strategic Planning
7.2.2 Organizational Readiness Assessment
7.2.3 Operational Planning
7.2.4 Project Team
7.2.5 Goal Setting
7.2.6 Program Design
7.2.7 Technology Review and Selection
7.2.8 Implementation Phase
7.2.9 Post-Implementation Phase
8 Functional Assessment and Activity Monitoring Technology Matrix Components
9 Contributors
9.1 Contributing Writers
9.2 Workgroup Members
9.3 Participating Vendors
10 Resources
1. Purpose of White Paper
1.1 Purpose
The purpose of this paper is to aid LeadingAge and other aging services organizations in understanding the range of Functional Assessment and Activity Monitoring Technologies available in the marketplace, their uses, and their benefits. It includes those that are wearable and aimed at consumers.
In addition, the portfolio will do the following:
- Help providers plan for, select, and implement these solutions.
- Include a Selection Matrix comparing existing Functional Assessment and Activity Monitoring solutions.
- Highlight an easy-to-use Online Selection Tool to help providers select solutions that best fit their requirements.
- Showcase a set of Provider Case Studies that highlight the impacts providers who implemented these technologies experienced, the challenges they overcame, the lessons they learned, and the advice they have for others.
This paper explains Functional Assessment and Activity Monitoring Technologies and their uses and benefits.
This information is meant to assist in understanding Functional Assessment and Activity Monitoring technologies, but it cannot possibly include all systems that may be available. Products mentioned in this report are only illustrative examples and have not been tested or independently evaluated or endorsed by LeadingAge or LeadingAge CAST. Please use this information as general guidelines in understanding functionalities and examples of current Functional Assessment and Activity Monitoring systems. Where appropriate, provider case studies were identified.
2 Functional Decline
2.1 Definition
According to the Functional Decline Chapter of the Aging Services Technology Study: Report to Congress,1 functional decline is “a complex process triggered by one or more underlying pathologies that leads to impairment or functional limitations, and that may ultimately result in disability and institutionalization.”
Many models help us understand age-related functional decline and loss of independence. One defines disablement as “the interaction of acute and chronic health conditions with environmental factors that advance or delay loss of function.”2Disability interferes with Activities of Daily Living (ADLs), such as eating, walking, dressing, and bathing.3 It also interrupts Instrumental Activities of Daily Living (IADLs) such as grocery shopping, housekeeping, financial management, and other activities needed for independent living.4
Functional decline is a broad term that can describe decreases in both physical and cognitive abilities and functionality. In this white paper, we focus on the physical aspects of functional decline. Health care professionals often assess physical decline in terms of certain markers, including decline in physical activity levels and generalized “wellness” that signal the onset or worsening of pathology, gait, and balance impairments that impact mobility and increase the risk of falls, and the ability to perform ADLs and IADLs that are necessary to maintain independence.
Functional decline can describe decreases in physical and cognitive abilities and functionality.
Identifying disability precursors early makes intervention easier. In addition, detecting events associated with functional decline or limitations quickly—such as falling—can greatly enhance the ability of health care professionals and family caregivers to effectively respond.
However, there are a number of specific challenges associated with addressing functional decline. Many of these issues stem from older adults, caregivers, and health care professionals being unaware of existing levels of function or of indicators of clinically meaningful changes in function. For example, older adults are frequently unaware of their level of activity, thereby making it difficult for them to determine if their level of function is declining. Similarly, caregivers of older adults may not notice that an older adult is walking less or with an unstable gait.
Other challenges associated with addressing functional decline involve the ability to generate ongoing information that is useful for decision making. For example, sleep disturbances can be a marker of functional decline, but it can be difficult for a remote caregiver to know that an older adult is experiencing disturbed sleep.5 Further complicating these issues are communications challenges among patients, caregivers, and health care professionals about functioning. Finally, it can be challenging to monitor the functioning of older adults if the technology require a high level of engagement to generate data.
2.1.1 Connection to Chronic Conditions, Cognitive Decline, and Lifestyle
Systematic literature review of longitudinal studies conducted between 1985 and 1997 was published in 1999. It found statistical associations between individual baseline risk factors and subsequent functional status in older people who lived in their communities.
The following factors, listed in alphabetical order, were most likely to cause a decline in functional status: Cognitive impairment, depression, disease burden (comorbidity), increased and decreased body mass index, lower extremity functional limitation, low frequency of social contacts, low level of physical activity, no alcohol use compared to moderate use, poor self-perceived health, smoking, and vision impairment. The review also revealed that past research has neglected some risk factors, such as nutrition and physical environment.6
2.2 Prevalence
According to the Aging Services Technology Study, many older adults have some difficulty performing ADLs.
- In 2007, one-quarter (25 percent) of Medicare recipients who live independently reported difficulty with one or more ADLs.
- Among older adults in community housing with services, 46 percent did.
- Among those in long-term care facilities, 83 percent did.
- Among older adults who live independently, an estimated 38 percent of older adults require assistive equipment such as walking or bathroom aids, 6 percent require personal assistance with ADLs, and 22 percent require both equipment and personal assistance for ADL performance.7
At age 65 and older, more than one-third of adults may risk loss of independence.
Independence may be at stake for more than one-third of adults age 65 and older; 38 percent report disabilities in areas such as ambulation and self-care. The number climbs with age. For adults aged 80 and older, 56 percent report severe disability, while 29 percent say they need help with ADLs.8
The risk for minority women over age 60 is especially high. Compared to their white counterparts, non-white women had poorer function in their lower extremities, greater difficulty performing ADLs, and a higher likelihood of walking with assistive devices.9
Functional decline can be more difficult to spot than changes in ADL performance due to incremental changes, which can be subtle, require frequent and detailed assessments that are not part of the standard of care, and can lead to more serious impairment.10 There are few reliable statistics on how gradual declines in activity and mobility—called antecedent conditions—may predict gross functional decline and eventual dependence.
Chronic conditions often cause functional decline in the U.S. For example, according to the 2007-2009 National Health Interview Survey (NHIS), approximately 50 million adults (22 percent) have been diagnosed with arthritis, which causes gait disorders, reduces mobility, yields other functional limitations, and causes an estimated 21 million people (9 percent) to limit their activities.11 Risk factors for falls include gait disorders and mobility limitations that increase the risk of stumbling, tripping, and losing balance.
Limitations can be especially serious when they occur along with other complex health issues associated with old age, such as loss of muscle mass, cognitive decline or impairment, poor eyesight, and neuropathy.12, 13 When older adults fall, they often fracture their hips. Broken hips are a leading cause of institutionalization in old age, especially among adults age 80 and older. As more people are aging and becoming functionally impaired, more technologies that prevent, detect, and mitigate functional decline and impairment become needed.
2.3 Cost and Burdens Associated
Along with functional decline and impairment come other burdens that occur more often as function decreases. According to the Functional Decline Chapter of the Aging Services Technology Study, Older adults point to good physical functioning as a key factor in maintaining a high quality of life.14 Those who rely on others for help with basic needs such as transportation or ADLs are more socially isolated, have poorer nutrition and exercise habits, and receive medical care less often than they need to.15
Functional decline and management takes an emotional and financial toll on family members.
Functional decline and management also takes an emotional and financial toll on family members who care for older adults and others with disabilities. Forty-three percent say they had no choice but to become caregivers, yet many are unprepared to handle these responsibilities on top of their jobs and their own household responsibilities.
Women carry an especially high burden, as they often provide a disproportionate amount of family caregiving, particularly among minorities. But a number of factors affect how big the caregiving burden is, including income, the caregiver’s age, the patient’s age, and severity of the patient’s disability.16 One study found a higher caregiving burden for patients who reported compromised ADLs. Caregivers struggling to provide transportation and financial management were likely to have the highest burdens and, in some cases, strong resentment.17
Estimated Costs
Caregiving may also lead to poverty in later life, according to some studies, because caregivers may not be able to earn as much and may need to tap their savings.18 In 2007, family caregivers provided an estimated $375 billion in unpaid health care and support to older adults with ADL or IADL limitations.19 These costs include time, transportation, lost wages, and decreased productivity, in addition to the emotional stress and worry.
- Costs vary depending on how close the caregiver and patient live to one another:
- Long-distance caregivers have $8,728 in out-of-pocket expenses per year.
- Caregivers who live with an older adult spend $5,885 per year.
- Those who live near the patient spend $4,570 per year.20
These costs are growing rapidly. The estimates exceeded $450 billion in 200921 and almost doubled to $522 billion in 2014, according to a more recent and more accurate estimate presented in a RAND Corporation study.22
Functional decline and impairment are a significant part of total health care spending, particularly among people with chronic diseases. A study conducted for the Office of the Assistant Secretary for Planning and Evaluation (ASPE) found these estimated costs in 2006 to be:
- $146 billion spent on functional limitations among community-dwelling residents (without comorbid chronic diseases).
- $236 billion spent on those who needed IADL and ADL assistance.
- $268 billion spent on assistance for other functional deficits.
Technologies that target functional decline and impairment are one strategy to bring about long-term care savings.
The same report found that functional limitations raise annual health care costs for adults with chronic conditions, no matter how many chronic conditions they have or the services they seek, such as emergency room visits, prescriptions, inpatient, and home health services.23 Average annual health care costs are much higher for older adults who need nursing home care than for those who live independently ($57,022 vs. $12,383 per person per year).
Covering the Costs
While some older adults turn to long-term care insurance to cover a portion of these expenses, the cost of these policies is rapidly rising beyond the reach of most people.24 Many people simply pay out of pocket for skilled nursing care or assisted living facilities until they exhaust their financial resources and transition to a Medicaid-covered facility.
In the future, the ability to receive long-term care may be more limited. Increases in the cost of services and coverage, the aging of the population, and the growing demand for health care services will place an unprecedented strain on Medicare, Medicaid, and health care providers. As a result, controlling costs while providing high-quality care will become even more important and will require especially innovative solutions.25
Because the costs of long-term care are so much higher than independent living, avoiding or delaying long-term care can yield significant reduction in costs.26 Technologies that target functional decline and impairment are one strategy to bring about these savings, as discussed in the Functional Decline Chapter of the Aging Services Technology Study: Report to Congress.
3 Definition/Types of Functional Assessment and Activity Monitoring Technologies (Non-Mutually Exclusive Categories):
3.1 Definition
Over time, several definitions of a functional assessment have evolved to match the changing needs of residents and the industry. A functional assessment is the process that captures and analyzes a person’s general behavior and capabilities to interact with the world, in order to determine his or her changing needs.
The general consensus, however, is that with an aging population the functional decline is implied more so than the possible improvement of an older adult’s ADLs and may include more granular assessments related to gait, balance, and grip strength, as well as broader types of activities like behaviors, sleep, social activities, etc.
3.2 Types of Functional Assessment
Functional assessments for an older adult encompass many aspects of daily living and can be grouped into two general areas: physical and cognitive.
- Physical Assessments: These cover sensory and mobility impairments: vision, hearing, gait, control over bodily functions, mobility, and ADL/IADL activities (bathing, dressing, and toileting).
- Cognitive Assessments: These cover behavioral changes, depression, memory decline, and general cognitive functions (recall, sequencing, multi-tasking).
It is important to note that, often, cognitive decline affects physical behavior changes and, therefore, a thorough and complete functional assessment should include physical as well as cognitive assessments.
Functional assessments should include physical and cognitive assessments.
A study by the Department of Epidemiology and Preventive Medicine at the University of Maryland, Baltimore found that “rather than simply being correlated markers of increasing frailty, cognitive and functional decline appear to influence the development of one another.”27
Functional decline can also be an early sign of cognitive decline, adding a time dimension to the cause and effect relationship between the two assessment types. A study on early detection techniques for Alzheimer’s involving 444 individuals over an average of six years found that “while memory loss is often one of the first symptoms of Alzheimer’s, those who developed Alzheimer’s experienced a decline in visuospatial skill three years before diagnosis.”28 Nine other studies conducted in the UK in 2011 found that executive function was associated with falls and gait speed slowing in older adults.29
3.3 Activity Monitoring Technologies
Assessing functional decline is a challenging process because decline is usually gradual and subtle and therefore involves a great variety of factors to consider. The relationship between cognitive and functional decline and general reluctance by the patient to acknowledge the decline also adds to the complexity.
Monitoring technologies have long represented a field of interest for health care professionals in that they promise a wealth of information and better focused and personalized care. Yet the broad adoption of these technologies requires a holistic approach that extends beyond the technology to address operational care, financial business models, and legal issues.
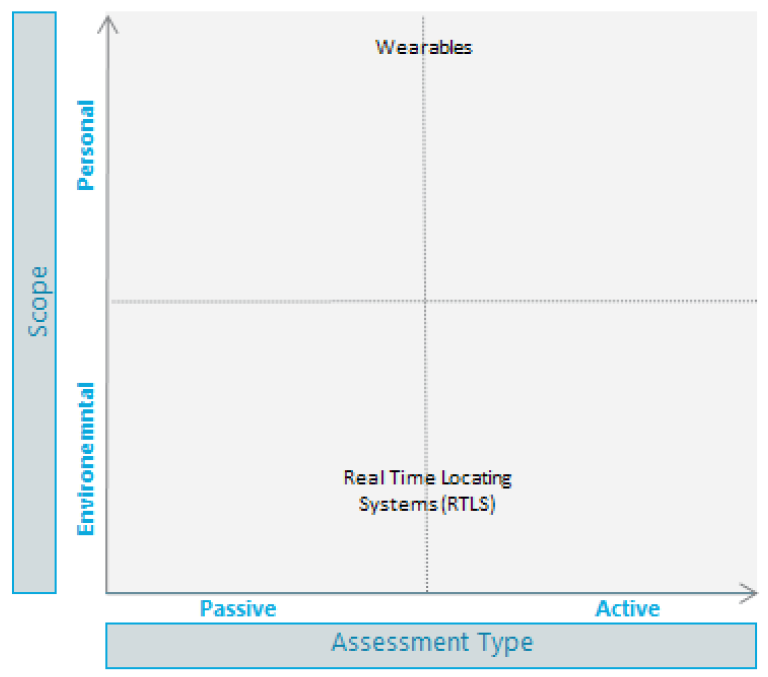
These technologies range from embedding sensors in the fixed environment to mobile, wearable, or personal devices and vary in the way the monitored individual interacts with them. Some are completely passive, and others require specific interactions with sensing devices and/or user interfaces.
3.3.1 Passive Monitoring Systems
3.3.1.1 “Smart” Environments
Completely passive environmental monitoring systems embed sensors in the environment and usually do not require the individual to do anything or wear any sensor or carry a specific mobile device. Smart environments are emerging after several similar but independent sensory objects were created over time, such as sensors for garages and windows, or the Nest thermostat. Today’s attempts at creating commercially viable smart objects leverage the interconnectivity of these objects. This development makes more comprehensive and targeted monitoring possible.
Today, complete systems provide wireless real-time monitoring capabilities, including location tracking for hospital, senior living, and facility-based settings. Some systems may also include pull cords, door systems, bathroom and hallway sensors, thermostats, and humidity sensors. Analyzing data gathered from these systems can provide a wealth of information, without requiring active input from the user.
Recently, mainstream consumer electronics companies joined the fray in offering integrated solutions to monitor environments. For example, Google announced in May 2015 the release of a new Android-based platform designed to be embedded in all home appliances. The company is joining the race to dominate the market and set its standards against Apple’s HomeKit and Microsoft’s HomeOS platforms. Senior living and post-acute care providers can use these solutions once they mature and include enterprise-level features such as security and centralized management.
3.3.1.2 Wearables
Devices that are carried or worn monitor the person rather than the environment around the person. Completely passive wearable devices do not require the user to enter any data or do anything special. They usually focus on improving or maintaining people’s well-being and encourage them to actively participate in their wellness.
However, wearables can gather trends and sudden events and communicate those to third parties, such as doctors or nurses. The proactive response can dramatically improve the person’s life. Personal data from multiple individuals can also be aggregated to provide population-level insights on interactions, if location information is considered, or may inform congregate-based interventions.
Active monitoring systems may require the person to go through a certain routine and/or input specific data.
3.3.2 Active Monitoring Systems
3.3.2.1 Environmental Assessments
Active environmental assessments use sensors in the environment, but they may require the monitored individual to go through a certain routine and/or input specific data. For example, some functional and activity monitoring systems that use Microsoft’s Kinect sensor bar may require the assessed individual to stand in a certain location, take a specific posture, and perform a certain sequence as prompted by a visual user interface.
3.3.2.2 Wearable-Based Personal Assessments
Again, active wearable monitoring systems may require the user to go through a certain routine and/or input specific data. For example, a wearable accelerometer-based system aimed at performing Timed Up and Go (TUG) assessment would require the user to indicate the start to the system and then perform the up and go test as instructed.
Another example is wearable activity armbands used for weight management that can calculate activity levels and caloric burn rate, but may require the user to input his or her daily caloric intake for the system to provide effective advice on the level of activity the person needs to engage in to maintain or lose weight. (See figure 1)
4 Potential Uses and Benefits of Functional Assessment and Activity Monitoring Technologies
4.1 Overview
The confluence of a rapidly growing senior population with the emergence of flexible, cost-effective sensors and platforms for technology applications has led to an unprecedented menu of technology options for older adults. We now have unique abilities to capture, analyze, and actively provide feedback on an older adult’s functional abilities and activities. The availability of these technologies and devices is changing the way care providers and residents/patients are managing their health, in several ways:
- Ongoing, Trended Data vs. Point-in-Time Assessments: Technology is allowing clinicians and other care providers to gain better insight into a patient’s ongoing health through not only biometrics such as blood pressure, heart rate, weight, and blood glucose, but also activities and behaviors. This insight comes from monitoring key data elements at more frequent intervals and trending that data over time. Wearable devices or products with sensors allow a person to collect health as well as wellness data at any time instead of only during the traditional, annual visit with clinicians.
- Early Identification & Risk Mitigation: In the new technology-enabled world, we are transitioning from incident management to health and wellness management and disease prevention. For example, identifying changes early, such as a change in gait or balance, allows us to intervene earlier and reduce the risk of a fall. Another example might include early identification of symptoms such as weight gain, or lab markers that can provide important information to a physician or caregiver to prevent an exacerbation of heart failure. The shift from pay for service to pay for performance as well as the shift of payer sources is accelerating this transition from reactive interventions to preventive, proactive, and management/maintenance interventions.
For the purpose of this white paper, we have limited the scope to devices and systems whose primary purpose is activity monitoring and functional assessment. There are other devices that also provide this type of information, but their primary purpose may be something else. Examples include connected clinical equipment such as a vital sign monitor that sends data directly to an electronic medical record, managing medications, etc. Those technologies are outside the scope of this initiative but may be covered by other CAST initiatives. Please see CAST’s Telehealth and RPM, Medication Management and EHRinitiatives.
In this report, we have included technology used to assess and monitor ADLs, IADLs, functional assessments, and other parameters.
Technologies can detect a change in activity levels, providing early notification for intervention.
4.2 Activities of Daily Living (ADL) Monitoring
Technologies available on the market today can monitor many ADLs, providing comprehensive information about a resident’s activity levels, capabilities, abilities to remain independent, or supportive services needed to remain independent. Through the use of such technologies, a family member or care provider can detect a resident’s activity levels or change in activity levels, providing early notification for intervention.
Motion sensors provide information that is meant to indicate a resident in motion, but limitations in the technology exist. For example, the lack of identification capability may not indicate if the activity is performed by the actual resident or by the staff or family that are caring for him or her.
Technologies available today can capture information when the toilet has been used. Examples include water sensors in the toilet or motion sensors that assume a resident is using the toilet. This information can be used to identify patterns such as increased toileting, which can be a leading indicator for urinary tract infections, allowing a caregiver to provide early intervention.
For a person experiencing incontinence who requires help and support with toileting, incontinence briefs with sensors can detect when voiding occurs and relay that information to a caregiver for assistance. It also can identify voiding patterns that may help caregivers provide assistance in toileting activities and reduce the negative consequences associated with incontinence. Bathing employs similar methods, through the use of water and motion sensors, or motion and humidity sensors, in the bathroom shower area.
Feeding can be inferred in several ways. Sensors can be installed in refrigerators or other appliances, food cabinets, utensil drawers, etc. that track each time a resident opens/closes the refrigerator door and infer that the resident ate.
Another form of technology called real-time location systems (RTLS) is able to track when a resident is in the dining room during lunch hours, again inferring a meal was eaten. Dressing can be monitored in a similar fashion, with sensors on the closet doors or dresser drawers that track when the doors are opened and closed.
Many social engagement technologies are designed specifically for older adults.
4.3 Instrumental Activities of Daily Living (IADL) Monitoring
Much investment is occurring today in technologies that enable and monitor IADLs. Closely linked to the ability to live and care for oneself independently, IADLs are also closely linked to a resident’s quality of life. The ability to detect early changes in behaviors such as isolation or the ability to prepare meals will enable early intervention to help prevent further decline in health and wellness, both physical and psychological.
- Social Interaction: Many social engagement technologies are being designed specifically for older adults, made to be user friendly and embedded in items they could use every day, such as the TV. Video chatting with family, social networking (Facebook or similar systems for older adults), and email/messaging systems that utilize voice recognition technologies rather than requiring typing are all available today.
Social interaction with other older adults can also be monitored. Real-time location systems let every individual carry a transmitter, typically designed as a bracelet, personal emergency response system (PERS) pendant, staff badge, visitor badge, and more. These systems can monitor when a resident is in the same room as other older adults, staff, doctors, or family members. Then caregivers know how much time the patient has spent engaging with others, inferring that social interaction is occurring when two people are in the same room.
This same inference can be used to show that a resident is participating in activities (i.e., present in the game room), having fun (i.e., showing up at the cocktail lounge during happy hour), and engaging in rehab (i.e., spending 90 minutes in the gym on Saturday, with a rehab therapist present for half an hour).
Several technologies can monitor telephone usage in the home in addition to checking on resident activity. This feature allows family members and care staff to see who is calling and to track social activities.
- Eating: Several of the social engagement and interaction technologies allow residents to pre-order food or room service using their tablets, mobile phones, or televisions. Some systems offer integration with menu and food management systems to manage allergies.
- Movement: Tracking of resident movements (i.e., left their home, drove 30 miles down the freeway, entered the vicinity of the mall) are also available via various GPS tracking devices. The devices can be embedded in shoes, clipped to belts, and worn as watches. They can track a resident’s movement and even send alerts when a resident leaves a pre-determined geographic area or geo-fence, such as a one-block radius around the community.
Many technologies are currently in active development, awaiting testing for deployment.
Future Technology
As the microchips, sensors, and the devices they drive become smaller, more energy efficient, and longer range, the ability to gather more useful information will continue to grow. Sensor technology has wide application today, but it’s not hard to imagine a day when the applications will expand and extend to capture more comprehensive, trended information.
Bathtubs and showers with water use indicators, refrigerators and cabinets with sensors to track opening and removal of food or beverages, devices that can detect and track falls more effectively, and other technologies are currently in active development, awaiting testing for deployment. Appliances, including refrigerators, ovens, washing machines, and others, are currently available with embedded sensors that show usage.
4.4 Functional Assessment
There are several types of systems that are focused on more global functional assessments, like balance, strength, and endurance. In what follows, we will discuss several areas of potential for physical functional assessments.
- Balance Assessments: There are several commercial balance assessment systems ranging from balance platforms to body or limb sensor systems. All of these perform a core assessment of functional balance including the Romberg test of balance and some form of a limit of stability test. In addition, some systems offer normative population data (based on age, gender, height and weight, and fall history) that allow the system to be used as a screening tool to identify potential fall risks.
Balance platform systems generally capture balance aspects by using a stable or unstable platform with sensors in the platform to measure the patient’s center of gravity (CoG) and micro-movements. An unstable platform will be raised 12-18 inches and will move under the patient to test and challenge his or her balance either in evaluation or in training. If it is a stable platform, the patient is low, one to two inches above the ground, and relies on patient movement rather than platform movement to both test and provide training to improve balance.
The other types of balance systems measure body sway or the limbs and include a gait element. These systems might have sensors placed around the ankles and waist, in the sole of a shoe, or in the patient’s socks. These systems can perform the same way as a stable balance platform system, but may also include a gait analysis and training component.
The gait training will give the therapist detailed measurements through a number of tests, including Timed Up and Go (TUG), velocity, cadence, stride length, left and right swing, stance, and timing of the different phases of the gait cycle. There is a large variance in the ease of use of the hardware and software, user interface, the type of and granularity of the data, and the way in which information is presented.
- Strength Assessments: There are several ways to measure and assess functional strength, ranging from Dynamometers and pinch gauges that measure hand strength to a full multi-piece strength equipment system that calculates an overall strength score based on a multi-factor assessment and use of a patient-specific ID system.
There are also individual pieces of equipment from which a therapist can infer functional strength. Examples include sit-to-stand exercisers, active/passive trainers, and unweighting systems. This equipment lets the therapist gauge strength in functional movements based on the amount of assistance the equipment provides, either through passive assistance or from unweighting the patient. Both strength systems and individual pieces that provide assistance can be used for assessment, strength building, and documenting functional strength improvement.
- Endurance: Very few technologies are used to measure cardiovascular endurance. Many paper-based protocols exist to translate a patient’s heart rate and performance on a piece of fitness equipment (treadmills, steppers, bikes, etc.) to assess cardiovascular endurance level.
Many functional assessment and activity monitoring technologies also monitor other health and wellness information.
4.5 Physical Activity and Other Parameters
Many functional assessment and activity monitoring technologies also monitor other health and wellness information. Wearable activity tracking technologies promote an active lifestyle, behavior change, and weight loss. Wearable sensors, such as wrist bands, clip-on devices, and shoes with embedded sensors offer variety and flexibility. However, function, form, and connectivity have not come together in a manner that is appropriate for all senior living settings.
- Ambulation: Many systems today are able to monitor ambulation (i.e., distance traveled, time spent walking, time of the day spent moving, speed, steps, etc.) through wearable devices that utilize an accelerometer or through motion sensors that detect movement in a resident’s room.
- Biometrics: Biometrics can be monitored through various technologies. Wearable devices are able to monitor heart rate. Mats can be placed under mattresses and monitor not only sleep, but also respiration and heart rate. Wearables come in the form of patches that can be affixed to the skin and monitor ECG, heart rate, heart rate variability, respiratory rate, skin temperature, activity (step count), posture, and fall detection, then send that information wirelessly to caregivers.
- Gait: Gait is one of several important factors in determining propensity for falling. The ability to detect changes in gait could provide caregivers with the information they need for early intervention before a fall actually occurs. Various systems can monitor gait. Some are currently invasive and not ideal for daily use. However, technologies exist that measure a patient’s gait, including acceleration, speed, balance, step-length, cadence, timing, foot pressure distribution, and posture.
- Falls: Wearable technology today allows for not only activity monitoring, but also personal emergency response and fall detection. Wearable technologies exist that blend personal emergency response, location tracking, activity monitoring, and wander monitoring detection to prevent the unsafe egress of patients with dementia or Alzheimer’s.
- Pressure Ulcers: Technology in beds and mattresses that monitor sleep can also monitor weight and pressure ulcer risk factors. These systems alert caregivers when a resident needs to be turned by monitoring the amount of pressure on the mattress, the movement of the resident, and the time that a resident has been still. This technology can also be used to determine if a patient intends to leave a bed, so that a caregiver can be alerted if the patient is at risk of falls.
Many of these systems include a host of other sensors to monitor the patient’s environment, such as whether the stove, lights, coffee maker, or other household appliances are turned on. They can monitor the presence of water, room temperature, and more.
The data collected can be viewed by care staff, family, and sometimes the doctors and patient.
4.6 Uses for the Information
The data streaming from these systems can be used for four primary purposes: care coordination, notification, trending, and sharing.
Much of the data collected by functional assessment and activity monitoring systems can be viewed by care staff, family, and sometimes the doctors and patient. This information sharing can ensure that each caregiver has the best and most comprehensive information available for care planning, coordination, and service delivery. The information can be used to update care plans and put early interventions in place.
These systems may signal an emergency where a patient may need immediate assistance.
Some of the information collected by these systems may signal an emergency where a patient may need immediate assistance—if a patient falls, doesn’t get out of bed, doesn’t leave the bathroom in one hour, etc. Alerts can be sent to care staff, family, or emergency service personnel as a phone call, text message, email, etc., depending on the care setting and service agreement. This alert can ensure that a patient receives the prompt attention needed.
Some of the information collected does not signify an imminent danger but can be collected, analyzed, and trended over time. This information can be used to identify trends in resident wellness (i.e., activity levels have been slowly declining for past 45 days) or to identify variations from normal trends (i.e., the patient typically uses the bathroom once in the middle of the night every night but used the bathroom four times each of the last two nights). This information can help caregivers provide early interventions, long before a resident may report the change. As a result, these early interventions can reduce the likelihood of costly care transitions.
Lastly, the information can be transmitted to other systems, such as electronic medical records or other clinical systems. This sharing ensures seamless coordination of care and puts the best information possible in the hands of all caregivers, helping to improve the potential care for the patient.
Coordination of information into a central system to deliver timely, consolidated, relevant, and actionable data to caregivers is critical to the success of these technologies. The ultimate goal is to have the right sensor technology integrated into software platforms, with big data analytics engines and proper internal processes to interpret reports and alerts that will allow family and care organizations to make more informed decisions to improve quality of care.
These technologies have benefits for physical activity, weight loss, falls reduction, alerting caregivers, and health care costs.
5 Benefits of Functional Assessment and Activity Monitoring Technologies
The literature shows several benefits of functional assessment and activity monitoring technologies when coupled with feedback and interventions aimed at changing behavior, professional care, and supportive services.
5.1 Active Lifestyle and Behavior Change
There is some question as to whether activity monitors can encourage people to be more active. The Aging Services Technology Study report cites a study that found participants who wore activity monitors as part of a physical activity program were more active after six months than control groups and were just as active as participants who received telephone-based counseling. After 12 months, the activity-monitoring and control groups were equally active, and the telephone group was more active.30
The results suggest that monitors can encourage more physical activity in the short term, but alone they may not support long-term behavior change. Further research may show ways to use monitors, possibly in combination with other forms of support, to increase physical activity over the long term.
5.2 Weight Loss and Combating Obesity
Obesity can lead to functional decline and impairment, and activity-monitoring technologies may be able to help. One study used activity monitors to measure caloric intake, physical activity levels, and energy expenditures in a group of diabetes patients participating in a 12-week exercise intervention. Participants lost weight, but because there was no control group, the findings are open to interpretation.31
Monitoring physical activity may help identify risks to independence early and prevent them.
However, another study showed that as daily steps increased, long-term risk for cardiac events decreased. These results suggest that monitoring physical activity can help identify risks to independence early and prevent them.32 Results also indicate that physical activity monitoring may be helpful even for adults who are healthy.33
5.3 Improving Gait and Reducing Fall Risk
As functional decline and impairment increase, so do falls. Technologies that detect and prevent falls, then, can help lower functional decline and impairment.
Monitoring foot pressure is the first step. Losing sensation in the feet can cause poor balance, slower and irregular gait, and increased fall risk.34 Older adults are particularly susceptible, especially those who have diabetes and neuropathic complications, and may find it hard to stay active.
A pressure-sensitive shoe insole can measure how pressure is distributed across the foot and detect balance problems related to functional decline. These devices also could issue alerts in response to foot pressure patterns that show the user is having trouble walking.35
Also under study are insoles that vibrate the feet to stimulate nerves and heighten sensation. One study found the vibrations made older adults sway less and feel steadier.36 Another study looked at insoles that generate impulses while the person walks. These sensors made older adults’ gaits more consistent, whether they had fallen or not. Therefore, this technology could benefit people with a history of falling and known functional decline.37
One study suggests these technologies can predict acute events.
5.4 Family Caregiver Engagement to Prevent Costly Transitions
Passive monitoring can have a psychosocial impact on patients and caregivers. A study followed patients and caregivers for four months. Neither group reported significant changes in quality of life. Even though more hours of caregiving were needed, caregivers did not report increased strain. The monitoring technology may have engaged family caregivers in the care process in ways that did not increase their perceived burden.
This study also suggests these technologies can predict acute events. Several patients showed a decline in functional status right before they were hospitalized, suggesting that passive-monitoring technologies may detect changes that in some cases could alert caregivers to intervene or could avoid crises and lower the likelihood of costly transitions to higher levels of care.38
Passive activity-monitoring systems may pay for themselves by preventing doctor visits, laboratory tests, and hospital stays.
5.5 Health Care Costs
The monthly costs of passive activity-monitoring systems vary, but in the long run, they may pay for themselves by preventing unplanned doctor visits, laboratory tests, and hospital stays.39 A study of three assisted living facilities reviewed the costs and benefits of passive monitoring over three months.40 Patients who were monitored had fewer emergency room visits and fewer hospital days than those who were not monitored, and their health care costs for billable services were much lower: monitored participants spent $17,407.02, including monitoring costs, and unmonitored ones accrued $67,753.88.41
A recent white paper supports this notion. A Philadelphia PACE (Program for All-Inclusive Care of the Elderly) program combined daytime remote monitoring with intermittent care and provided an alternative to nursing homes that was supportive but cost less.42
In another study, diabetes patients answered daily health questionnaires online. A case manager would receive and review the data online and contact a physician if symptoms warrant clinical intervention. Patients said their quality of life was better and they needed services less, such as inpatient, emergency room visits, post-discharge and outpatient visits. They also noted small improvements in physical health assessments.43
The question of whether these systems are good for maintaining functional abilities is still unanswered. The research is encouraging, but it is not definitive.
Medicare, Medicaid, and private health insurance usually do not cover these services.
6 Potential Long-Term and Post-Acute Care (LTPAC) Provider Business Models
6.1 Medicare, Medicaid, and Private Health Insurance Coverage
Generally speaking, Medicare, Medicaid, and private health insurance do not cover functional assessment, activity monitoring, telecare, or related supportive services.
6.1.1 Program of All-Inclusive Care for the Elderly (PACE)
PACE (Program of All-Inclusive Care for the Elderly) is a Medicare and Medicaid program that helps people meet their health care needs in the community instead of going to a nursing home or other care facility. PACE organizations provide care and services in the home, the community, and the PACE center. They have contracts with many specialists and other providers in the community to make sure that patients get the care they need.44
PACE focuses on individual enrollees, who have a team of health care professionals working with them and their family to make sure they get the coordinated care they need. Many PACE participants get most of their care from staff employed by the PACE organization in the PACE center. PACE centers meet state and federal safety requirements.
Because PACE providers operate under a capitated payment model and are at risk for all care costs, including hospitalization and nursing home costs, they have a vested interest in controlling costs and flexibility in covering traditionally uncovered benefits. This may encourage PACE providers more than their traditional fee-for-service counterparts to adopt and utilize functional assessment, activity monitoring, telecare, and telehealth to deliver health care and supportive services.
6.2 Medicaid Waiver Coverage
Medicaid waivers are vehicles states can use to test new or existing ways to deliver and pay for care services in Medicaid and CHIP. There are four primary types of waivers and demonstration projects:
- Section 1115 Research & Demonstration Projects: States can apply for program flexibility to test new or existing approaches to financing and delivering Medicaid and CHIP.
- Section 1915(b) Managed Care Waivers: States can apply for waivers to provide services through managed care delivery systems or otherwise limit people’s choice of providers.
- Section 1915(c) Home and Community-Based Services Waivers: States can apply for waivers to provide long-term care services in home and community settings rather than institutional settings.
- Concurrent Section 1915(b) and 1915(c) Waivers: States can apply to simultaneously implement two types of waivers to provide a continuum of services to the elderly and people with disabilities, as long as all federal requirements for both programs are met.45
Pennsylvania is the only state that currently covers functional assessment, activity monitoring, telecare, and related supportive services.
According to a CAST Analysis of Medicaid Waiver Programs, Pennsylvania is the only state that currently covers functional assessment, activity monitoring, telecare, and related supportive services. In fact, Pennsylvania has the most comprehensive coverage for aging services technologies in its telecare program, which includes home telehealth, activity/wellness monitoring, medication dispensing, and personal emergency response systems (PERS); please see CAST Analysis of State Payment for Aging Services Technologies (ASTs).
6.3 Potential Affordable Care Act (ACA) Opportunities
The Affordable Care Act (ACA) is shifting the health care system in the U.S. away from the traditional fee-for-services to a pay-for-performance system. Moreover, CMS is moving to reimburse Medicare Certified Home Health based on a value-based purchasing model instead of a Prospective Payment Model. This shift is starting to put more emphasis on proactive and preventive care and eliminate the misalignment of incentives inherent in traditional Medicare, Medicaid, and private insurance programs with respect to functional assessment, activity monitoring, telecare, or related supportive services.
The ACA includes many provisions that might encourage adoption of remote activity monitoring, telecare, telehealth, and RPM technologies and services.
There are a few provisions and models in the ACA that would benefit from, provide opportunities to cover, and consequently encourage the supportive services and related assessment and monitoring technologies.46 The act created the Center for Medicare & Medicaid Innovation (CMMI), which is tasked with exploring new care delivery and payment models and initiatives47 that do the following:
- Use more holistic, patient-centered, and team-based approaches to chronic disease management and transitional care.
- Improve communication and care coordination among care providers.
- Improve care quality and population health while reducing growth in expenditures.
The act puts explicit emphasis on the use of technology in general and health information technology (health IT) in particular, including Health Homes for Enrollees with Chronic Conditions, the Independence at Home Demonstration, and the Use of Technology in New State Options for Long-Term Services and Supports.48
These initiatives include the following:
- Hospital Readmission Reduction Program (HRRP).49
- Accountable Care Organizations (ACOs).50
- Bundling of Payments models, of which the following two are relevant to Long-Term and Post-Acute Care (LTPAC) providers:
LTPAC providers bring a significant value for hospitals, physician groups, payers, and ACO partners by providing the following services:
- Rehabilitation and skilled nursing facilities provide post-discharge/post-acute patient rehabilitation.
- Skilled nursing facilities, assisted living facilities, continuing care retirement communities, housing with services, and home health agencies provide post-acute patient stabilization and sub-acute chronic disease management.
- LTPAC provides holistic person-centered care, including support services.
- LTPAC offers lower cost care settings than hospitals.
These new care delivery and payment models will enable LTPAC providers who use technologies like functional assessment, activity monitoring, and telecare, and who provide proactive supportive services, to derive revenue sources from strategic partners. The white paper, titled The Importance of Home and Community-Based Settings in Population Health Management, offers some key questions LTPAC providers should discuss with their acute care partners.53
Private payers may be another payment source for technology-enabled supportive services.
Another payment source for functional assessment, activity monitoring, telecare, or related supportive services may be private payers or out of pocket.
6.5 Standard of Care and Other Payment Sources
LTPAC and community care providers, special population agencies, self-pay and self-insured organizations, and others, especially not-for-profits, may offer or cover an array of functional assessment, activity monitoring, telecare, or related supportive services. These services may be covered by grants or offered as standard of care. The organization may absorb the cost or different revenue sources, including charitable contributions, may cover it.
6.6 Return on Investment (ROI) of Telehealth and RPM
Return on investment (ROI) represents the ratio of the net gains relative to the initial investment over a certain period of time. Subsequently, ROI can be expressed in the following equation:
As discussed above, functional assessment, activity monitoring, telecare, and related supportive services deliver various benefits, including potential financial savings to different stakeholders, including patients and/or their families, payers, care providers, etc.
ROI depends on the care delivery model, the payment/reimbursement model, the technology, and costs.
However, the financial savings and ROI depend on a number of factors, including the care delivery model, the payment/reimbursement model, the technology, and of course costs. The first and most important step in calculating ROI is to consider the different stakeholders, identify the investors, and calculate the gains and savings netted/accrued to each investing stakeholder under each particular care delivery and payment model.
When calculating ROI, one should only include the gains that accrued to that particular stakeholder minus all expenses, relative to that stakeholder’s own investment/cost. Often the reduction of hospital days is erroneously included in the providers’ ROI, which is not true under the traditional fee-for-service reimbursement model and can be misleading. Such a reduction usually accrues to the payer.
6.6.1 ROI to Patients and/or Their Families
ROI to patients and/or their families can be calculated as follows:
For private pay patients and their families, for example, the financial gains of functional assessment, activity monitoring, telecare, or related supportive services lie in prolonging independence by maintaining activity and wellness, which may prevent disability, and avoiding the need to move into assisted living or skilled nursing facilities. These benefits are significant.
The gains may also include savings in co-pays for recurring hospital visits, and of course a higher quality of life, which is difficult to quantify. The patient’s and family’s expenses are the monthly out-of-pocket costs of private pay for functional assessment, activity monitoring, telecare technologies, or related supportive services, plus any co-pay for the occasional physician office visit, lab tests, and prescriptions.
6.6.2 ROI to Payers
ROI to payers can be calculated as follows:
For dual Medicare and Medicaid eligible patients who are nursing home eligible, for example, the financial gains of home functional assessment, activity monitoring, telecare technologies, and related supportive services under a Medicaid Waiver program that accrue to Medicaid depend on keeping patients in their own homes with home care and other supportive services. Otherwise, Medicaid would be liable for the costs of nursing home room and board. Medicaid’s investment is the monthly rate of home telecare technologies and additional supportive services aimed at keeping the patient independent.
In this particular example, there may be additional savings, like reductions in hospitalization and hospital readmission costs that accrue to Medicare, which is liable for and covers health care costs. Consequently, such savings or gains should not be included in calculating Medicaid’s ROI, which in this case is investing in the telecare technologies and supportive services.
The care provider who makes investments in technology may reap lower costs and higher reimbursements.
6.6.3 ROI to Care Provider
ROI to care providers can be calculated as follows:
The care provider who makes investments in information and communications technology infrastructure, telecare technology, and care services may reap the following benefits:
- Lower costs in delivering the same services, including staff efficiencies and staff travel costs (if the payer covers the remote services, rather than just the in-person visit).
- Higher reimbursements/payment from the payer or strategic partner in terms of incentive payments for avoiding more costly care settings, procedures, events, or penalties.
For example, an LTPAC provider partnering with a physician group ACO to manage a chronically ill patient population can potentially get a percentage of the incentives or shared savings payments the ACO receives from the payer for reducing hospitalizations and hospital readmissions, which can be significant for certain populations.
- The LTPAC provider’s net gain:
- +
The sum of all gains accruing to the LTPAC provider in staff efficiencies, increased referrals from the ACO, traditional fee-for-service payments, and additional incentive payments received from the ACO.
–
Minus the costs of leasing the home telecare equipment and actual costs of services delivered. - The physician group ACO’s ROI:
+
The portion of the payer’s incentive payment that they get to keep plus any additional fee-for-service payments due to more frequent office-based services.
–
Minus the actual costs of services they deliver (for example, in medication reconciliation or care coordination), relative to the portion of incentives they pass through to the LTPAC provider.
A contrast is a partnership between an LTPAC provider and hospital under the traditional fee-for-service model. For example, the LTPAC provider may help its hospital partners reduce 30-day readmission rates for pneumonia, congestive heart failure, and heart attack, helping the hospital avoid Medicare’s payment penalties under the Hospital Readmissions Reduction Program.
For example, the hospital may contract with and pay the LTPAC provider a percentage of the penalties saved for delivering telecare and supportive services that reduce 30-day readmissions for patients discharged from the hospital after being admitted for one of the above-mentioned three conditions.
- The LTPAC’s net gain:
+
The sum of all gains accruing to the LTPAC provider in staff efficiencies, increased referrals from the hospital, traditional fee-for-service payments, and additional payments received from the hospital.
–
Minus the costs of leasing the home telecare equipment and actual costs of services delivered. - The hospital’s ROI:
+
The portion of avoided penalties it gets to keep, plus any additional fee-for-service payments it gains for more referrals due to improved quality ratings.
–
Minus the actual costs of services the hospital delivers, relative to the portion of avoided penalties it passed through to the LTPAC provider, plus any additional costs incurred for staff time in care coordination, medication reconciliation, or health information exchange.
6.6.4 Online ROI Calculator
Once individual investors have been clearly identified, an estimate of the ROI to the different stakeholders can be calculated. The SCAN Foundation has recently published a white paper on making the business case for person-centered care with instructions for using an ROI calculator they developed.73
This return on investment (ROI) calculator is designed to quantitatively assess the business case for person-centered care (PCC) programs that serve older adults with chronic conditions and functional limitations. PCC programs are ones where individuals’ values and preferences are elicited and, once expressed, guide all aspects of their health care, supporting their realistic health and life goals. This type of care is achieved through a collaborative relationship and decision-making process among the person, their chosen supports, and their medical and social service providers. As discussed in detail above, the business case for PCC involves weighing the costs of offering this approach to care against the benefits expressed in dollar terms. Benefits accrue principally in the form of avoided medical utilization, but also potentially in the form of higher revenues.
The ROI calculator has a number of practical features:
- Risk Stratification: The population that is suitable to receive PCC can be segmented into high and moderate risk categories. The ROI will be likely higher (i.e., a higher percentage) for the segment that is at higher risk for medical utilization. The calculator can show how limited the offering must be if a specific return were being sought. Potential Revenue from PCC: The calculator allows for PCC program offerings to incorporate possible revenue enhancements in addition to the more probable benefits resulting from reducing costs.
- Slider Bars: This feature allows the user to compute instantaneous “what-if” calculations by changing values of inputs and immediately viewing these new inputs’ influence on the ROI.
- Flexibility in Expressing Variables: All variables can be entered by the user in terms of their convenience – per person, per month, or per year. Hospital admissions, for example, are generally reported on an annual basis whereas encounters with a social worker or nurse practitioner are often expressed on a monthly basis. The calculator automatically converts rates and volumes, no matter how expressed, into a common per member per month (PMPM) measure.
- Scenarios: This feature allows ROI comparisons across different programs as well as varied constellations of input values. For example, the user can create optimistic and pessimistic scenarios and compare the results. Sometimes even the pessimistic scenario can yield an acceptable result for the ROI.
- Accounting for Uncertainty: Admittedly, some key determinants of the ROI are not known with certainty. Therefore, a “Monte Carlo” simulation that accounts for uncertainty with respect to the magnitudes of key variables is an optional part of the tool. This simulation recognizes this uncertainty and displays accordingly a reasonable range of results for the ROI rather than a single deterministic value. The tool also quantifies the strengths of the separate influences each variable has on the resulting ROI.
- Other Metric – Payback Period: In addition to the ROI result, the calculator displays the payback period – defined as the number of months the PCC program would need to operate (assuming a positive operating margin) for any initial investment to be recouped. This metric may be useful for programs involving substantial up-front launch costs.
- Threshold Analysis: The tool provides the ability to conduct threshold analysis, whereby the user can query the calculator on questions such as the following: What is the maximum amount that can be spent on PCC so that the program does not lose money? Or for a given cost of delivering PCC, how effective must it be in reducing certain events (e.g., hospital readmissions) in order to generate a required (hurdle) level of ROI?
To access the calculator tool, go to The SCAN Foundation.
7 Planning for and Selecting Appropriate Functional Assessment and Activity Monitoring Technology
To consider any new enabling technology, the Information Technology (IT) Department must align with its internal customers’ goals and objectives. It must also be familiar with the end users of the technology and their objectives and goals. Organization leaders must include IT leadership in the strategic planning process and articulate the organization’s strategic plan. In carrying out the plan, project teams must include IT personnel to communicate needs and capabilities and to coordinate the organization’s goals with the technology selected.
By being able to describe a “typical” set of technology users and older adults served, the IT team can better decide on the program’s set-up and features.
By being able to describe a “typical” set of users of the technology and a “typical” set of resident or older adult the organization serves, the IT team can better decide on the program’s set-up and features. Keeping in mind the needs and goals of the organization and its customers as the strategy is carried out is important as the project evolves over time.
The following questions can serve as a guide to developing the technology strategy and plan:
- What are the organization’s overall strategic goals and objectives?
- How does the functional assessment and activity monitoring technology being examined fit into those goals and objectives?
- What is the organization looking to improve related to 1) performing functional assessment of patients/ residents/ clients and 2) new functional assessment and activity monitoring technology?
- What exists within the organization for this purpose now?
- How will the new functional assessment and activity monitoring technology be used over the next year? Three years? Five years?
- What are the related, priority operational issues that concern leadership?
- What are the organizational capabilities as they relate to functional assessment and activity monitoring technology?
- What business processes need improvement before functional assessment and activity monitoring technology is implemented?
- What key indicators will leadership use to assess performance with functional assessment and activity monitoring technology?
- Does the leadership team have ready access to key indicator information or does it require building something new?
- Are there any issues related to privacy/security, regulatory, reimbursement/payment, and competitive landscape in relation to functional assessment and activity monitoring technology?
Clarity on these points provides direction so the technology plan can ultimately support and enable the organization as a whole. For additional resources pertaining to Strategic Planning and Strategic IT Planning, please review the CAST Strategic IT Planning Tools.
7.1 Understanding the Setting, Population, and Issues
7.1.1 Gemba Rounds
Gemba is a lean management term, meaning the real place where value is created. The Gemba is where leaders go to observe and understand the real work, bringing management to the front line.54
Observing the Gemba objectively is an easy approach to creating a picture of the current processes, population, and issues. Observations should be conducted as a first step and without interfering in the observed activities. It can be most effective when conducted by both those who work in the environment and those who do not. Including resident observations in this process can round out perspectives and provide opportunities for a person-centered care approach when applicable. Following up on observations with focused interviews can fill the gaps where processes are not clear or not observable.
The observation process and subsequent interviews should focus on the purpose of the project and systems that touch it.
The observation process and subsequent interviews should focus on the purpose of the project and systems that touch it.
- How is functional assessment and/or activity monitoring currently carried out?
- What tools are used, when and by whom?
- What factors influence the way you conduct the assessments and their outcomes and how?
- What systems touch the processes and where might they be improved?
The answers provide an understanding of the current process, existing gaps, and improvement opportunities, which can affect future elements, such as introducing a new technology. This process also provides clarity on what form of functional assessment and activity monitoring is needed, what tools might best fit the need and environment, and whether there is staff with time and skills to deliver, assess, and respond to the assessments.
Observing from within can address whether there are tools and space enough in the environment to administer testing. Observing interpersonal interactions provides cultural insight as well. Is staff open to change, and what sort of change management processes might work best within the environment and culture?
It is not uncommon after conducting observations to note where current processes can and should be improved before introducing new assessments. For example, if the staff is consistently pressed for time, an evaluation of workflow can be done to examine where work might be redistributed or streamlined, leaving all staff more time to conduct detailed functional assessments.
7.1.2 Systems Thinking
Key to observation is the understanding that behavior is influenced by the system in which it occurs.55 For example, addressing reductions in patient falls includes examining the system that influences that effort, including staffing levels, medication, the environment, patient call technology, general staff knowledge, and the accountability for responding to residents.
Looking only at the behavior of an individual providing care is of limited effectiveness in addressing a specific problem. It is the work of the leaders in the organization to take the first steps in the process of examining the system as a whole and disseminate the understanding of what influences the target issue.56
The vision provides guidance about what core values to preserve and where to encourage change.
7.2 Planning for Functional Assessment and Activity Monitoring Solutions
Great organizations understand the difference between what should never change and what should be open for change. This rare ability to manage continuity and change—requiring a consciously practiced discipline—is closely linked to the ability to develop and follow a vision. The vision provides guidance about what core values to preserve and where to encourage change.57
7.2.1 Visioning and Strategic Planning
- Objective: Involving the organization in collectively creating an image of the desired future state to guide strategy and planning.
- Key Deliverables: A clear, engaging vision to guide the organization’s mission.
Visioning can be defined as the process of forming a mental image of the future in order to make plans, set goals, and undertake activities. While mission statements guide the organization in its day-to-day operations, visions provide a sense of direction for the long term—the means to the future.58
A vision statement for an organization should include the organization’s:
|
Strategic planning is proactive and long-range and addresses an issue for the organization moving towards the mission and vision. For the purpose of this paper, the issue is the ability to conduct functional assessment and activity monitoring (See Figure 2). After the vision is set, the process of strategic planning generally follows these steps:60
- Determine the gap between current state and the vision.
- Set a direction, including baseline goals, to close the gap.
- Implement the strategic plan.
- Evaluate the strategic plan periodically.
For additional resources pertaining to strategic planning and strategic IT planning, please review the CAST Strategic IT Planning Tools.61
7.2.2 Organizational Readiness Assessment
- Objective: To identify the current state of the organization and barriers to success.
- Key Deliverables: Presenting assessment findings to the team to elicit a concrete plan for managing obstacles.
Sydney J. Harris is quoted as saying, “Our dilemma is that we hate change and love it at the same time; what we really want is for things to remain the same but get better.” Wanting change is one thing; being ready to implement and accept change is quite another. The concept of readiness itself is controversial. “How ready is enough? Ready in whose eyes?” asks Combe.62
If organization leaders are unprepared, it would follow that so is the rest of the organization.
Cullen and Adams, in their article Planning for Implementation of Evidence-based Practice, suggest that while “expectations for evidence-based healthcare [increases], the most difficult step in the process, implementation, is often left to busy nursing leaders who may be unprepared for the challenge.”63 In the conduct of functional assessment and activity monitoring, those nursing leaders often are the organization. If organization leaders are unprepared, it would follow that so is the rest of the organization.
Rantz et al., provide a list of readiness indicators based on their findings, which include the following:
- Learning: A willing leadership team (for example a nursing home administrator or director of nursing) interested in learning how to use their federal quality improvement/quality management (QI/QM) reports as a foundation for improving resident care and outcomes.
- Change Champions: One or more of the leaders who are willing to be a change champion and others make sure that current QI/QM reports are consistently printed (using the recommended six-month default date) and shared with each nursing unit monthly.
- Inclusiveness: Leaders willing to involve all staff in the facility in educational activities to learn about the QI/QM process and the reports that show how their facility compares with others in the state and nation.64
Part of assessing readiness to change and implement the key principles is to ask the following:
- How does your staff currently view their role in making improvements?
- What is your current approach to making improvement?65
The IT team can assist leadership in moving toward readiness by providing unbiased communication of their views on the challenges and capabilities of the technology options and throughout the implementation process.
7.2.2.1 Considerations for Resident/ Client-Facing Solutions
Considerations for resident/client-facing solutions must include a number of assessment categories. The first three should be considered for both care providers and residents:
- Assessment of issues and needs.
- Assessment of competencies and abilities.
- Assessment of personal preferences.
- Provider services and responsibilities.
- Ability to pay.
Lack of awareness of existing technologies, the value and utility of these technologies, and how to acquire and use them is present among older adults. It also exists in all levels of caregiver and health care professionals, despite their role as trusted referral channels and influential change agents.66
Within the evaluation process, the following considerations should be made in relation to the available technologies:
- Stigma: Stigma associated with some Aging-Services Technologies (ASTs) on the part of older adults and individuals with disabilities causing issues with adoption.
- Privacy and Security: Issues related to privacy and security act as barriers to ASTs for all stakeholders.
- Usability: Usability is critical to encouraging widespread adoption of ASTs.
- Liability: The belief (whether true or false) that ASTs could increase liability exposure must be managed.
- Integration: Integrating ASTs with health IT, which can cause disruptions in provider workflow and changes to interoperability between ASTs and health IT.
- Costs: Reimbursable costs of the ASTs or the related professional services delivered.
- Evidence: The existence (or lack) of scientific evidence supporting the ASTs, which may act as a barrier to selection of, adoption and/or reimbursement of use.67
Before selecting the technology, assess the knowledge, skills, and abilities of staff who would use it.
7.2.2.2 Staff Competencies
Before selecting the functional assessment and/or activity monitoring technology, assess the knowledge, skills, and abilities of staff who would use it. The selection committee must consider the effort, costs, and time needed to train staff to ensure it chooses a technology that will be implemented and adopted successfully. For example, if the staff is generally uncomfortable with technology, introducing a system requiring complex data entry may not be a good fit. For staff with more advanced capabilities, systems that do not include adequate results reporting may cause frustration.
7.2.2.3 IT Infrastructure
Assess current IT capabilities and existing programs. The technology industry is pursuing a number of strategies to address interoperability. Evaluate existing technologies for their ability to integrate with any potential technologies to be added. This includes allowing information and messages to be exchanged seamlessly between systems. For more information, please see the IT Infrastructure Section of CAST’s Strategic Planning and Strategic IT Planning workbook.
7.2.2.4 Operating Environment (including Applicable Federal and State Regulations)
Observations must include an assessment of how the current environment addresses metrics, protocols, and procedures, including those related to government regulation. Training must accompany any new technology that includes new metrics or affects protocols and procedures. Staff must know the new process for getting reports and use the date to change processes and improve quality. Continuous involvement in quality improvement helps users own the process and take responsibility for the change.
7.2.3 Operational Planning
- Objective: Create a detailed plan to address the needs required to meet the organization’s strategy.
- Key Deliverables: The future organization’s design; detailed plan to close gaps in current versus future organization and project charter.
The first step in this process is to review and confirm the strategic plan and review the findings from the operational readiness assessment. The team should document the gaps between the desired objectives and the current status of the organization.
During the operational planning step, the team will answer this question: “How do we get there?”
The team should maintain a list of open issues and risks for any items they are not able to resolve. During the operational planning step, the team will answer this question: “How do we get there?” The team responsible for this activity will design the future organization by considering the following:
- People: Do we need to train and grow current team members? Do we need to add additional staff to the team? Are additional skill sets needed for the future organization?
- Process and Workflow: Do we need to optimize or change clinical and business workflows to support the strategic objectives? Are new workflows required?68
- Technology: What enabling technologies, both in terms of applications and infrastructure, are required to support the future organization? What security measures need to be in place to meet privacy requirements?
- Regulatory: What regulatory changes are in process that may affect the organization?
- Quality: What is needed to support industry guidelines and directives?
The answers will form the basis of the project charter, which will guide the project team and ensure alignment with strategic objectives.
The project charter is defined as follows: “A document issued by the project initiator or sponsor that formally authorizes the existence of a project and provides the project manager with the authority to apply organizational resources to project activities.”69 It incorporates the following:
- Project objectives.
- Project team composition and skill sets.
- Financial analysis, including ROI.
- Plan to address changes in the organization.
- Communication plan – What are we doing?70
- Education – Why are we doing it?
- Training – How do we do it?
- Plan to address regulatory and security requirements.
- Key activities and deliverables.
- Risks and risk mitigation plan.
Once the operational planning phase is complete and approved, the organization moves to the next activity for creating the project team.
7.2.4 Project Team
- Objective: Create a cross-functional team to execute the project.
- Key Deliverables: Project team, high-level project plan, project kickoff.
Based on the needs identified in the project charter, the organization will create a project team. Successful design and implementation requires a cross-functional team and project stakeholders. The most successful programs include the organization’s day-to-day operations and involve all staff.
The new care delivery model requires involvement from executive leadership, clinical teams, technical representatives, durable medical equipment/logistics, finance, operations, risk management, compliance, training, and marketing/business development. The project team should have a project manager responsible for overall project activity, communication, and coordination.
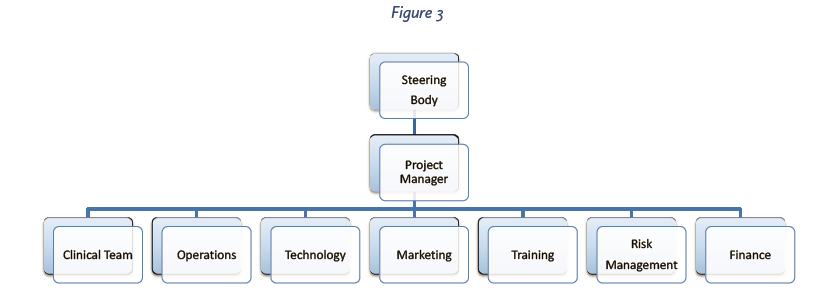
The project team will create a project plan consistent with the project charter and formally kick off the project. The project team will educate the organization on the objectives of the project and the high-level timeline and milestones to ensure success.
7.2.5 Goal Setting
- Objective: Identify and document project goals.
- Key Deliverables: Approved, measureable goals with baselines, targets, a plan to measure, and a reporting plan.
The project team will use the objectives outlined in the project charter and develop goals for the project. Many goal setters recognize the S.M.A.R.T. model (Specific, Measurable, Achievable, Relevant, and Time-bound) as an established framework for creating goals.71
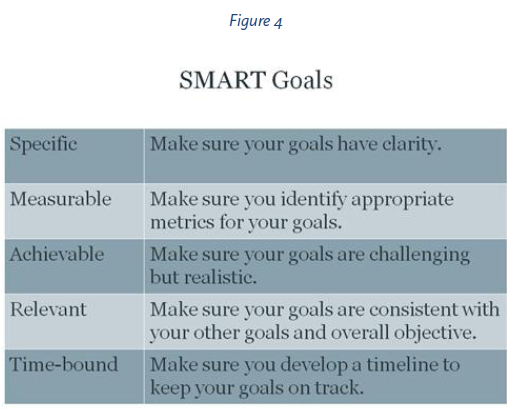
A goal-setting worksheet is provided in the toolkit from CMS under the Quality Assurance & Performance Improvement (QAPI) program.72 Goals should be monitored and evaluated over time. The project team should document baseline data, measure progress toward the goals, evaluate goals, and validate the ongoing relevance of the goals over time.
Goals for each organization are unique and may incorporate ideas from the following categories:
- Clinical Outcomes: Chronic conditions, readmissions, adverse events.
- Satisfaction Outcomes: Patient satisfaction scores, employee scores.
- Operational Outcomes: Staff productivity, response times.
- Financial Outcomes: Occupancy, prevention vs. treatment, new offerings.
7.2.6 Program Design
- Objective: Develop detailed requirements for the project.
- Key Deliverables: Detailed requirements, vendor candidates.
The project team will develop a set of detailed requirements to support the next activity, technology review and selection. The goal of this activity is to create a list of criteria to evaluate potential partners for the technology solution required to support the organization’s strategy and objectives.
The key to successful program design is to develop a closed-loop solution with metrics to provide accountability.
The key to successful program design is to develop a closed-loop solution with metrics to provide accountability. The program needs to align with the organization’s strategy.
Programs should be designed with the organization’s short- and long-term goals in mind to help ensure success. Care coordination, collaboration, and communication with other care providers to enhance patient care and outcomes should also influence the program design. The design of each program should always align objectives, strategies, and technical plans with care partners by using technology to supply information and facilitate communications, as well as any patient monitoring solutions. Be sure to share experiences from similar organizations to assist in building a new program or strengthening an existing one. Please see the companion case studies that CAST is collecting.
The detailed requirements will span a variety of topics and include the following:
- Care Setting(s).
- Care Workflow: Plus processes and protocols.
- Quality Measure Requirements.
- Regulatory/Security/Privacy: FDA, HIPAA, HITECH Act, etc.
- Technology Standards: Corporate IT standards hardware/software, Local vs. SaaS.
- Reporting Needs.
- Integration Requirements: Electronic Health Records (EHRs), Admit/Discharge/Transfer (ADT), nurse call, Personal Emergency Response Systems (PERS), communication systems, telehealth devices, alarm/wandering systems, medication management systems, internal data reporting solutions.
- Training: Plus support, documentation, and upgrades.
- Installation and Implementation Services: Clinical, technical, regulatory.
- Communications: Alerts, messages, escalations, status.
The project team will document detailed requirements for the items above. In addition, the team will document any initial vendor names for the next phase pf the project, technology review and selection.
7.2.7 Technology Review and Selection
- Objective: Perform a comprehensive review of market solutions, identify finalists, and select a primary and back vendor partner.
- Key Deliverables: Vendor selection scoring matrix, due diligence (demonstrations, site visits, reference checks), pilot plan, cost analysis.
The technology review and selection phase uses the design requirements from the program design phase and compares them to vendor solutions to identify potential vendor partners to support the program’s goals and organization’s needs. It includes five steps (See Figure 5).
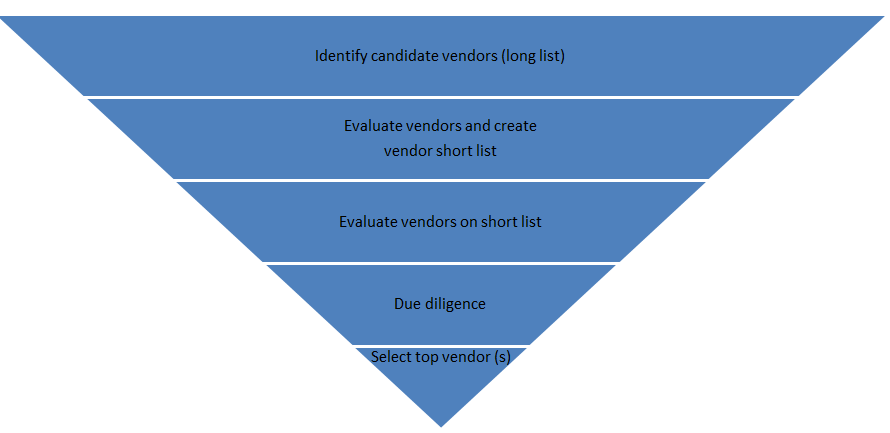
Step 1: Identify Candidate Vendors: There is a wide selection of offerings and vendors for solutions in functional assessment and activity monitoring technologies. The first step will be to identify the long list of potential partners and short list criteria. Key resources for creating the initial vendor list include the following:
- CAST Functional Assessment and Activity Monitoring Online Selection Tool.
- CAST Functional Assessment and Activity Monitoring Matrix.
- CAST website, online discussions, and associates.
- Recommendations from colleagues.
- LeadingAge conferences.
- Trade publications.
- Vendor comparison reports.
- Webinar sponsors.
Step 2: Evaluate Vendors and Create Vendor Short List: The team can use the CAST Online Selection Tool and “short list” criteria. The criteria include the highest priority/must-have requirements for the organization to evaluate vendors and refine the list to three to five potential partners.
Step 3: Evaluate Vendors on Short List:
- Create a Request for Proposal (RFP) for the vendors to submit: During the RFP process, providers are encouraged to interview prospective vendors; engage representatives from the clinical team, management, finance, and IT; and use objective metrics to compare proposed vendor solutions. We encourage you to check provider case studies with the vendors, including those collected by CAST.
- Develop use cases and conduct face-to-face or online meetings to review how the vendor solution handles the use cases: A cross-functional team should review the vendor response as a group and have a rating or scoring system available to conduct the evaluation.
- Review a mix of both the RFP and use case: In this step, the project team creates a hybrid of the above two processes. Use case reviews may be focused on the highest priority use cases.
Step 4: Due Diligence: The project team will recommend a technology solution at the end of this phase and will ensure all recommended partners have been vetted for the following:
- Financial and business stability.
- References from existing customers, including customer visits.
- Validation of support, training, software maintenance, documentation.
- Validation of regulatory and security components – FDA, HIPAA, HITECH ACT.
- Peer review via CAST and other industry organizations.
- Confirmation of detailed initial and ongoing costs.
- Integration capabilities.
Step 5: Select top vendor(s): Based on the evaluation steps above, the team will identify the recommended vendor partner and, if possible, a backup vendor. The solution may require two or more complementary vendors to meet the program’s requirements. The recommendation should include objective evaluation ratings, cost comparisons, and any other criteria the selection team deems to be important differentiators.
The project team should submit or present their recommendations with the goal of getting approval to pilot or implement the solution.
7.2.8 Implementation Phase
- Objective: Create a cross-functional project team and execute the project.
- Key Deliverables: Established project team, project plan, project kickoff, detailed design, pilot, go live.
Once the technology vendor(s) solution has been identified and approved and the project has been funded, the implementation phase begins. The project team will form, the project team will create a detailed project plan, and the project will kick off.
- Agree upon Project Scope and Goals: The project implementation team should be a patient-centered interdisciplinary team consisting of the following, at a minimum: physicians, nurses, pharmacists, IT, and, if appropriate, residents/ patients/ families. Develop a project plan identifying milestones, resources, tasks, and timeline.
- Outline Project Tasks. Project tasks include mapping clinical and business processes and developing new processes and procedures. They should not be confined to the functional assessment processes in the setting. The implementation team is patient-centered so the focus should also be on the patient’s journey. The patient’s journey/ transition through care settings needs to be part of the mapping. Otherwise, we create a system that is focused on one setting or limited from the perspective of services that could be delivered to support independence.
- Set Leadership: The project manager will have overall responsibility for the project and will manage scope, costs, timelines, resources and communications, and issues and risks. Implementation projects contain a number of interrelated and parallel activities that can be represented by individual team leads. A central planning and reporting tool or dashboard can be used to keep the project team, stakeholders, and staff informed and coordinated.
- Create a Detailed Design: The project team’s first step will be to create a detailed design of the solution using the technology vendor’s solution. Document new processes, metrics, protocols, and procedures. Capture any issues, gaps, or risks. During this part of the project, the team will develop high-level approaches for change management, reporting, security, and meeting regulatory requirements.
- Develop and Configure: During this activity, the project team will create the solution configuring the software, developing required integrations and procuring and setting up the required hardware. Detailed schedules and plans will be created for change management, security setup, report design and access, and regulatory compliance.
- Test and Pilot: This activity will include detailed testing of the functionality, training, security rollout, and report validation. The organization may choose to evaluate the solution at an initial pilot site to validate the design and ensure the requirements for achieving the stated goals are met. The pilot activity can be the final user acceptance test, or a separate user acceptance test can be conducted prior to going live.
Once testing, training, and validation are complete, the team can prepare for going to live production. - Go Live: During the go live phase, the solution is turned on and handed over to the end users. Live integration, alerts, and reporting will be active. The project team should be prepared for initial support requests, clarifications, and issues capture and resolution.
7.2.9 Post-Implementation Phase
Once the project is complete, monitoring and evaluation are important functions to see if the project goals, identified in the goal setting phase, were achieved.73 The transfer of knowledge from the implementation team to those who will be using the system is critical for the system’s sustainability. Refresher training and an internal user group ensure that users are aware of the system’s new features and functionality as they are developed. A clinical and financial analysis should be done post implementation to see if the goals of the project were attained.
End user champions are key to the ongoing success of the solution. Identifying best practices and reporting enhancements and success stories also help to maintain momentum during the initial rollout and beyond. The project team may also leverage tools to ensure workflow and clinical processes are improving.74
A project review should be conducted to capture lessons learned, open issues, and identify next steps.
8 Functional Assessment and Activity Monitoring Technology Matrix Components
CAST’s Functional Assessment and Activity Monitoring workgroup, consisting of providers, vendors, and consultants, compiled a list of functional assessment and activity monitoring products that serve the LTPAC market, as well as a list of functionalities and capabilities that would help providers choose the product that best fits their business line and functional requirements.
Each functional assessment and activity monitoring vendor was then provided the opportunity to complete a self-review of the workgroup’s pre-determined questions. Some of these vendors chose not to participate. Those who did participate were then invited to nominate a case study from a provider’s perspective on the use of the vendor’s product. The Functional Assessment and Activity Monitoring Selection Matrix includes the following information:
Business Line/Care Applicability
Business line/care applicability illustrates the various business lines to which the functional assessment and activity monitoring product is applicable, including the following:
- Acute Care Settings (Physicians’ Offices, Emergency Department, Hospitals, Attending LTPAC Physician)
- LTPAC and Other Settings (Home Health/Home Care, Hospice, Housing with Services, Community-Based Programs, Adult Day Care/Senior Centers, Assisted Living Facilities, Acute Rehab Facilities, Long-Term Acute Care Hospitals, Long-Term Care Rehab Facilities, Skilled Nursing Facilities, Intermediate Care Facilities, Memory Care Facilities, Intellectual Disabilities/Mental Retardation/Developmental Disabilities (ID/MR/DD) Facilities, Continuing Care Retirement Communities (CCRC), Program of All-Inclusive Care for the Elderly (PACE), Accountable Care Organizations (ACO)/Integrated Delivery Networks (IDN), Multiple Site Integration)
System Type
System type illustrates the different user types from the assessed patient/resident/client/user’s perspective to which a product is applicable, including the following:
- Mobile-Fixed (Wearable, Handheld, Sensors Embedded in Object(s), Desktop Computer/ Appliance, Kiosk, Sensors Embedded in the Environment)
- Passive-Interactive (Completely Passive: No Intentional Interaction with Sensors & No Input through User Interface Required, Quasi-Passive: No Intentional Interaction with Sensors, but Requires Input through User Interface, Quasi-Interactive: Requires Specific Intentional Interaction with Sensors, but No Input through User Interface, Fully Interactive: Requires Specific Interaction with Sensors, AND Requires Input through User Interface)
- Single/Multi User (Single User, Multi-User without Capacity to Distinguish Users, Multi-User with Capacity to Distinguish Users)
Program Development and Support Offered
This category includes options for the following:
Program Development (Planning, Business Model Templates, Workflows, Change Management, etc.)
- Care Staff Engagement
- Clinician Engagement Services
- User Education
- User Engagement
- Family Engagement
- Other (Please List)
Activity of Daily Living (ADLs)
This category includes the options for the following ADLs and the sensor(s)/method for which the activity is recorded:
- Bathing
- Eating
- Dressing
- Toileting
- Ambulation
- Grooming
- Transferring (To or from bed, chair, toilet, or shower)
Instrumental Activities of Daily Living (IADLs)
This category includes the options for the following IADLs and the sensor(s)/method for which the activity is recorded:
- Ability to Use Telephone
- Shopping
- Food Preparation
- Housekeeping/Cleaning
- Laundry
- Responsibility for Medication
- Managing Money
- Other
Physical Activity
This category includes the options for the following Physical Activities and the sensor(s)/method for which the activity is recorded:
- Overall Activity
- Steps
- Distance
- Flights of Stairs
- Gait Acceleration
- Gait Speed
- Step Length
- Stride Length
- Balance
- Shuffling
- Up and Go Test
- Cadence
- Sleep Stages
- Sleep Length
- Total Time in Bed
- Active Calories
- Other
Other Parameters
This category includes the options for the following Other Parameters and the sensor(s)/method for which the activity is recorded:
- Biometric (Heart Rate, Respiration, Blood Pressure, Blood Oxygen, Weight, Fluid Intake, Other)
- Risk Assessments (Fall Detection, Fall Prevention, Pressure Ulcer Detection, Pressure Ulcer Prevention, Wander Management)
- Environmental (Environmental Parameters; etc. High or Low Temp, Environmental Control; etc. Turn on/off an Appliance)
- Wellness (Health/Wellness Questionnaire, Daily Check-In)
- Other (Please List)
Sensor to HUB Communication
This category includes the options for the communication type between the sensors to the HUB. The options include the following:
- Wired
- Wireless (Wi-FiZigBee, X10, Propriety Alarm Protocol, Bluetooth (No, Yes; Standard Bluetooth, Yes; Bluetooth LE, Yes; Both), Other)
Front-End Hardware Unit Patient/Client/Resident/User Interface & Communications
This category includes the following options:
- Login Modality, Please list if applicable (e.g., scan card, PIN)
- Touch Screen
- Audible Prompts
- Visual Prompts
- Haptic Prompts
- Low Vision Support
- Customizable Questionnaires
- Thresholds Are Customizable
- Branching Logic Based on User’s Responses
- Communications Modality (Plain Old Telephone System (POTS) Line, DSL Internet Connectivity, High-Speed Internet Connectivity, Wi-Fi Connectivity, Cellular Connectivity, Minimum Internet Connectivity Speed Required)
Hardware and Software Requirements – Front End
These requirements list the required desktop/laptop specifications for Software-Only Solutions, including requirements for the following:
- Minimum Processor Speed, Hard Drive Storage, RAM requirements if applicable
- Operating System (OS) – Windows
- Operating System (OS) – Apple
- Operating System (OS) – Unix/Linux
Other features compared include the following:
Figure
Lastly, mobile options are listed as the following:
- Cellular Carriers that Support Solution
- Mobile OS – Android
- Mobile OS – Blackberry
- Mobile OS – iOS
- Mobile OS – Unix/Linux
- Mobile OS – Windows and/or
- Mobile-Optimized Interface (through dedicated app or mobile-optimized web pages)
Finally, we added a tab for any Additional Notes on hardware and software requirements.
Front-End Unit Support
This category includes the following options:
- Educational Self-Management Materials (On-Screen Educational Self-Management Material, Self-Management Educational Audios, Self-Management Educational Videos)
- Front-End Unit Multi-Language Support (English, Spanish, Mandarin, Cantonese,
- Korean, Russian, French, German, Hindi, Urdu, Portuguese, Arabic, Hebrew, Other (please specify))
- Remote Updates
- Remote Configuration Capability
Report Access
This element includes whether the following reports/records can be the following:
- Customizable Alert Thresholds
- Customizable Reports
- Ability to Schedule Automatic Reports
- Report Access Provided to the Following External Parties (User’s Physician, User’s Nurse/Other/Licensed Clinician,User Care Manager/ Professional Caregiver, Home Care Staff, Family, Other)
Alerts
This category includes the following options:
- Real-Time Alerts
- Call Center Support (Multiple Languages)
- Alerts Can Be Sent to the Following External Parties (User’s Physician, User’s Nurse/Other Licensed Clinician, User Care Manager/Professional Caregiver, Home Care Staff, Family, Other)
- Alerts Sending Modality (Pager, Telephone; Voice Messages, E-Mail, Text Message, Other)
Interfacing, Integration, and Add-Ons
This section looks into the functional assessment and activity monitoring solution’s integration capabilities with the following:
- EHR (Electronic Health Record)/PHR (Personal Health Record)
- Telehealth
- Medication Adherence Monitoring Dispensers
- Safety Monitoring Systems (e.g., Personal Emergency Response Systems (PERS))
- Printing Supported
- Dashboard Views
- Analytic Tools; Please List (e.g., Care Management, Predictive Analytics)
- Explain Integration Modality, Please List (e.g., Single Sign-On (SSO), LDAP)
- Other
Program Support Services
This category includes options for the following:
- Equipment Deliver/Pick Up
- Site/Home Installation
- IT/Network Troubleshooting & Support
- Front-End System Set-up
- Front-End System Customization
- Back-End System Set-up
- Back-End System Customization
- Onsite Staff Training
- Online Staff Training
- Onsite User Training
- Online User Training
- Equipment Cleaning
- Equipment Refurbishing
- Other
Interoperability, Interoperability Standards, and Certification
This section begins with type of interoperability and exchange capabilities supported, which include the following:
- None, Export Data Only, Import Data Only, or Bi-Directional Data Import and Export
This section also includes options for the following:
- Supported Interoperability Standards (HL7 Functional Assessment Questionnaire Framework, Other)
- Back-End HER/PHR Certification ((2014 ONC-ATCB Certification (Complete (please provide link); Modular (please provide link); No)Plan on pursuing ONC’s proposed voluntary certification?))
- Front-End System Certification (Continua Health Alliance Certified)
Care Supportability
This category includes options for the following:
- Phone Support–No, Yes (limited hours), Yes (24 hours)
- Web Support–No, Yes (limited hours), Yes (24 hours)
- E-Mail Support
- Listserv and/or Usergroup
- Online Training
- Onsite Training
- Other
Technical Supportability
This category includes options for the following:
- Phone Support–No, Yes (limited hours), Yes (24 hours)
- Web Support–No, Yes (limited hours), Yes (24 hours)
- E-Mail Support
- Listserv and/or Usergroup
- Online Training
- Onsite Training
- Other
- Warranty Information (Length of Product Warranty, Parts, Parts & LaborParts, and In-Field/On-Site Labor)
Legal/Regulatory/Cyberliability
This area touches on the following:
- FDA Clearance/ Listing – Cleared, Listed (this category may include Medical Device Data System (MDDS)), Pending, or None
- FDA Classification (Class I, Class II, etc.)
- HITECH
- HIPAA
- Security – List HIPAA & HITECH Act Requirements Met
- List Applicable Regulatory Requirements Met
- Provide a Link to Company’s Cyberliability Policy
- List Any Other Legal Requirements
- Provide Link to Sample Contract
Hardware and Software Requirements – Back End
These requirements list the required desktop/laptop specifications for Software-Only Solutions, including requirements for the following:
- Minimum Processor Speed, Hard Drive Storage, RAM requirements if applicable
- Operating System (OS) – Windows
- Operating System (OS) – Apple
- Operating System (OS) – Unix/Linux
Other features compared include the following:
Figure
Last, mobile options are listed as the following:
- Cellular Carriers that Support Solution
- Mobile OS – Android
- Mobile OS – Blackberry
- Mobile OS – iOS
- Mobile OS – Unix/Linux
- Mobile OS – Windows and/or
- Mobile-Optimized Interface (through dedicated app or mobile-optimized web pages)
Finally, we added a tab for any Additional Notes on hardware and software requirements.
Company’s Experience and Viability
- This area includes the following:
- Number of Years in Business
- Release Date of Current Version
- Number of Patients Served
- Core Customer Base/Focus of Line of Business
- Links to Additional Case Studies
The last section of the matrix is dedicated to the following:
- Strengths
- Areas for Improvement
- Ongoing Development
- References
9 Contributors
9.1 Contributing Writers
Majd Alwan, LeadingAge CAST
Scott Code, LeadingAge CAST
Moulay Elalamy, Benchmark Senior Living
Mike Hanson, BAM Labs, Inc.
John Rydzewski, Direct Supply Inc.
9.2 Workgroup Members
Majd Alwan, LeadingAge CAST
Kimberly Berger, Alarm.com
Kenny Chan, Kin On Health Care Center
Scott Code, LeadingAge CAST
Kaitlin Cuffe, Alarm.com
Dusanka Delovska-Trajkova, Ingleside at King Farm
Moulay Elalamy, Benchmark Senior Living
Mike Hanson, BAM Labs, Inc.
John Hoffler, Lutheran Social Ministries of New Jersey
Olga Jewusiak, Caremerge
Sarah Jones, Healthsense
Jeffrey Kaye, Oregon Health & Science University
Myron Kowal, Response Care Inc.
David Morgan, Graceworks Lutheran Services
John Rydzewski, Direct Supply Inc.
Michael Skaff, Masons of California
Kian Saneii, Independa
Jon Sanford, Georgia Tech
Frank Soltys, Felician Village
Rick Taylor, Silversphere
Dale Weaver, Brethren Village
9.3 Participating Vendors
Sixteen vendors, including 7 CAST Partners, Supporters and Business Associates participated in developing the Functional Assessment and Activity Monitoring Technology Portfolio. These included:
- LeadingAge Gold Partner with CAST Focus PointClickCare, Ricardo Meirelles
- LeadingAge CAST Supporter iN2L, Josh Hansen
CAST Business Assocaite participating in the portfolio included:
- Healthsense, Sarah Jones
- Jintronix, Mark Evin
- K4Connect, Martha Bader
- Response Care, Inc., Myron Kowal
- RF Technologies, Laurence Yudkovitch
Other participating vendors included:
- Biosensics, Ashkan Vaziri
- CarePredict Inc., Greg Zobel
- Claris Companion, Geof Auchinleck
- Curo Technologies, Steve Hopkins
- EarlySense, Maayan Wenderow
- IDEEA by MiniSun, Ming Sun
- Kinesis Health Technologies, Barry Greene
- StepWatch by modus, Blake Gudel
- Vigil Health Solutions, Troy Griffiths
10 Resources
1. Functional Decline Chapter. Report to Congress: Aging Services Technology Study. June 2012. Available at:https://aspe.hhs.gov/basic-report/report-congress-aging-services-technology-study Last accessed: July, 22, 2015.
2. Verbrugge, L.M., Jette, A.M. (1994). The disablement process. Social Science & Medicine, 38(1), 1-14.
3. Katz, S., Ford, A.B., Moskowitz, R.W., Jackson, B.A., Jaffe, M.W. (1963). The index of ADL: A standardized measure of biological and psychosocial function. Journal of the American Medical Association, 185(12), 914-919.
4. Lawton, M.P., Brody, E.M. (1969). Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist,9(3), 179-186.
5. Martin, J.L., et al. Sleep Quality in Residents of Assisted Living Facilities: Effect on Quality of Life, Functional Status, and Depression. Available online at: http://onlinelibrary.wiley.com/doi/10.1111/j.1532-5415.2010.02815.x/abstract?userIsAuthenticated=false&deniedAccessCustomisedMessage. Last accessed: July, 22, 2015.
6. Stuck, A.E., et al. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Available online at: http://www.ncbi.nlm.nih.gov/pubmed/10075171. Last accessed: July, 22, 2015.
7. Federal Interagency Forum on Aging-Related Statistics (2010). Older Americans 2010: Key indicators of well being. Hyattsville, M.D.: National Center for Health Statistics. Available online:https://agingstats.gov/docs/PastReports/2010/OA2010.pdf. Last accessed: August 22, 2015.
8. Administration on Aging (2009). A profile of older Americans: 2009. Washington, D.C.: U.S. Department of Health and Human Services. Available online at: https://aoa.acl.gov/Aging_Statistics/Profile/2009/docs/2009profile_508.pdf.
9. Ostchega, Y., Harris, T.B., Hirsch, R., Parsons, V.L., Kington, R. (2000). The prevalence of functional limitations and disability in older persons in the U.S.: Data from the national health and nutrition examination survey III. The Journal of the American Geriatrics Society, 48(9), 1132-1135.
10. Rantz, M.J., Aud, M.A., Alexander, G., Wakefield, B.J., Skubic, M., Luke, R., Anderson, D., Keller, J. (2008). Falls, technology, and stunt actors: New approaches to fall detection and fall risk assessment. Journal of Nursing Care Quality, 23(3), 195-201.
11. Centers for Disease Control and Prevention (2011). National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. U.S. Department of Health and Human Services.http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Last accessed: August 22, 2015.
12. Alexander, N.B., Goldberg, A. (2005). Gait disorders: Search for multiple causes. Cleveland Clinic Journal of Medicine,72(7), 586, 589-90.
13. Menz, H.B., Lord, S.R., St. George, R., Fitzpatrick. R.C. (2004). Walking stability and sensorimotor function in older people with diabetic neuropathy. Archives of Physical Medicine and Rehabilitation, 85(2), 245-252.
14. Webb, E., Blane, D., McMunn, A., Netuveli, G. (2011). Proximal predictors of change in quality of life at older ages. Journal of Epidemiology and Community Health, 65(6), 542-547.
15. Prinz, L., Cramer, M., Englund, A. (2008).Telehealth: A policy analysis for quality, impact on patient outcomes, and political feasibility. Nursing Outlook, 56(4), 152-158.
16. National Alliance for Caregiving and AARP (2009). Caregiving in the U.S.: A focused look at those caring for someone age 50 or older. Available online at: http://www.caregiving.org/data/FINALRegularExSum50plus.pdf. Last accessed: August 22, 2015.
17. Razani, J., Kakos, B., Orieta-Baralace, C., Wong, J.T., Casas, R., Lu, P., Alessi, C., Josephson, K. (2007). Predicting caregiver burden from daily functional abilities of patients with mild dementia. Journal of the American Geriatrics Society, 55(5), 1415-1420.
18. Wakabayashi, C., Donato, K.M. (2006). Does caregiving increase poverty among women in later life? Evidence from the Health and Retirement Survey. Journal of Health and Social Behavior, 47(3), 258-274.
19. AARP (2008). Valuing the invaluable: The economic value of family caregiving, 2008 update. Available online at:http://assets.aarp.org/rgcenter/il/i13_caregiving.pdf. Last accessed: August 22, 2015.
20. AARP (2008). Valuing the invaluable: The economic value of family caregiving, 2008 update. Available online at:http://assets.aarp.org/rgcenter/il/i13_caregiving.pdf. Last accessed: August 22, 2015.
21. Feinberg, L., Reinhard, S.C., Choula, R. Valuing the Invaluable: 2011 Update-The Growing Contributions and Costs of Family Caregiving. AARP Public Policy Institute. Available online at: http://assets.aarp.org/rgcenter/ppi/ltc/i51-caregiving.pdf.Last accessed: 23 July 2015.
22. Chari, A.V., Engberg, J., Ray, K., Mehrotra, A. The Opportunity Costs of Informal Elder-Care in the United States: New Estimates from the American Time Use Survey. Health Services Research (HSR), v. 50, no. 3, June 2015, p. 871-882. Available online at: http://www.rand.org/pubs/external_publications/EP66196.html. Last accessed: 23 July 2015.
23. The Lewin Group(2010). Individuals living in the community with chronic conditions and functional limitations: A closer look. Assistant Secretary for Planning and Evaluation. Washington, D.C.: U.S. Department of Health and Human Services. Available online at: http://aspe.hhs.gov/daltcp/reports/2010/closerlook.htm. Last accessed: August 22, 2015.
24. Kaiser Commission on Medicaid and the Uninsured (2006). Frontline perspectives on long-term care financing decisions and Medicaid assets transfer practices. Available online at: https://www.kff.org/medicaid/report/frontline-perspectives-on-long-term-care-financing/. Last accessed: August 22, 2015.
25. Crossen-Sills, J., Toomey, I., Doherty, M.E. (2009). Technology and home care: Implementing systems to enhance aging in place. Nursing Clinics of North America, 44(2), 239-246.
26. Federal Interagency Forum on Aging-Related Statistics (2010). Older Americans 2010: Key indicators of well being. Hyattsville, M.D.: National Center for Health Statistics. Available online at:http://www.agingstats.gov/agingstatsdotnet/Main_Site/Data/2010_Documents/Docs/OA_2010.pdf. Last accessed: August 22, 2015.
27. Black, S.A., Rush, R.D. Cognitive and functional decline in adults aged 75 and older. J Am Geriatr Soc. 2002 Dec; 50(12):1978-86.
28. Alzheimer’s Association, Research Highlights (2014). Available online at:http://alz.org/research/downloads/Research_Highlights.pdf. Last accessed: August 22, 2015.
29. Kearney F.C , Harwood R.H, Gladman J.R.F , Lincoln N., Masud T. The relationship between executive function and falls and gait abnormalities in older adults: a systematic review. Available online at: http://www.ncbi.nlm.nih.gov/pubmed/23712088. Last accessed: August 22, 2015.
30. Napolitano, M.A., Borradaile, K.E., Lewis, B.A., Whiteley, J.A., Longval, J.L., Parisi, A.F., Albrecht , A.E., Sciamanna, C.N., Jakicic, J.M., Papandonatos, G.D., Marcus, B.H. (2010). Accelerometer use in a physical activity intervention trial. Contemporary Clinical Trials, 31(6), 514-523.
31. Jung , J.Y., Han, K.A., Kwon, H.R., Ahn, H.J., Lee, J.H., Park, K.S., Min, K.W. (2010). The usefulness of an accelerometer for monitoring total energy expenditure and its clinical application for predicting body weight changes in type 2 diabetic Korean women. Korean Diabetes Journal, 34(6), 374-383.
32. Sisson, S.B., Camhi, S.M., Gurch, T.S., Tudor-Locke, C., Johnson, W.D., Katzmarzyk, P.T. (2010).American Journal of Preventive Medicine, 38(6), 682-683.
33. Jakicic, J.M., Davis, K.K., Garcia, D.O., Verba, S., Pellegrini, C. (2010). Objective monitoring of physical activity in overweight and obese populations. Physical Therapy Reviews, 15(3), 163-169.
34. Priplata, A.A., Patritti, B.L., Niemi, J.B., Hughes, R., Gravelle, D.C., Lipsitz, L.A., Veves, A., Stein, J., Bonato, P., Collins, J.J. (2006). Noise-enhanced balance control in patients with diabetes and patients with stroke. Annals of Neurology, 59(1), 4-12.
35. Trafton, A. (2006). Balance problems? Step into the iShoe: MIT grad student’s invention could one day prevent falls. MIT News. Available online at: http://web.mit.edu/newsoffice/2008/i-shoe-0716.html. Last accessed: August 22, 2015.
36. Priplata, A.A., Niemi, J.B., Harry, J.D., Lipsitz, L.A., Collins, J.J. (2003). Vibrating insoles and balance control in elderly people. Lancet,362(9390), 1123-1124.
37. Galica, A.M., Kang, H.G., Priplata, A.A., D’Andrea S.A., Starobinets, O.V., Sorond, F.A., Cupples, L.A., Lipstiz, L.A. (2009). Subsensory vibrations to the feet reduce gait variability in elderly fallers. Gait & Posture, 30(3), 383-387.
38. Alwan M., Leachtenauer J., Dalal S., Mack D., Kell S., Turner B., Felder R. (2006). Psychosocial impact of passive health status monitoring on informal caregivers and older adults living in independent senior housing. 2nd Institute of Electrical and Electronics Engineers Conference on Information & Communication Technologies: From Theory to Applications, 808-813.
39. Glascock, A., Kutzik, D. (2006). The impact of behavioral monitoring technology on the provision of health care in the home. Journal of Universal Computer Science, 12(1), 59-72.
40. Alwan, M., Sifferlin, E.B., Turner, B., Kell, S., Brower, P., Mack, D.C., Dalal, S., Felder, R. (2007). Impact of Passive Health Status Monitoring to Care Providers and Payers in Assisted Living. Journal of Telemedicine and E-Health, 13(3), 279-286.
41. Alwan, M., Sifferlin, E.B., Turner, B., Kell, S., Brower, P., Mack, D.C., Dalal, S., Felder, R. (2007b). Impact of Passive Health Status Monitoring to Care Providers and Payers in Assisted Living. Journal of Telemedicine and E-Health, 13(3), 279-286.
42. Business Wire (2010). New study finds remote monitoring technology enables the elderly to remain independent longer, reduces care costs for providers. Business Wire. http://www.businesswire.com/news/home/20100929005411/en/Study-Finds-Remote-Monitoring-Technology-Enables_Elderly. Last accessed: August 22, 2015.
43. Cherry, J.C., Moffatt, T.P., Rodriguez, C., Dryden, K. (2002). Diabetes disease management program for an indigent population empowered by telemedicine technology. Diabetes Technology and Therapeutics, 4(6), 783-791.
44. PACE Program, Center for Medicare and Medicaid Services (CMS). Available online at: https://www.medicare.gov/your-medicare-costs/help-paying-costs/pace/pace.html. Last accessed: July, 15 2015.
45. Medicaid Waivers Information, Medicaid. Available online at: http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/Waivers.html. Last accessed: August 22, 2015.
46. The Importance of Home and Community Based Settings in Population Health Management, Philips White Paper, March 2013. Available online at:http://www.leadingage.org/uploadedFiles/Content/About/CAST/Resources/The_importance_of_home_and_community_March_2013.pdf.Last accessed: August 22, 2015.
47. CMMI Innovations Models and Initiatives, CMMI, CMS. Available online at: http://innovation.cms.gov/initiatives/index.html.Last accessed: August 22, 2015.
48. Technology Related Provisions in the ACA, LeadingAge CAST. Available online at:http://www.leadingage.org/uploadedFiles/Content/About/CAST/Policy/Provisions_Relevant_to_Aging_Services_Technologies_HR_3590.pdf.Last accessed: August 22, 2015.
49. Medicare Hospital Readmission Reduction Program, CMS. Available online at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Last accessed: August 22, 2015.
50. CMS ACO Initiatives, CMMI, CMS. Available online at: http://innovation.cms.gov/initiatives/aco/. Last accessed: August 22, 2015.
51. Retrospective Acute Hospital Stay plus Post-Acute Services Payment Bundling Demonstration, CMMI, CMS. Available online at: http://innovation.cms.gov/initiatives/BPCI-Model-2/. Last accessed: August 22, 2015.
52. Retrospective Post-Acute Care Only Payment Bundling Demonstration, CMMI, CMS. Available online at:http://innovation.cms.gov/initiatives/BPCI-Model-3/. Last accessed: August 22, 2015.
53. Cohen, N., van de Craen, D., Stamenovic, A., Lagor, C. The Importance of Home and Community-Based Settings in Population Health Management. Philips Home Monitoring. March 2013. Available online at: https://www.leadingage.org/sites/default/files/Provisions_Relevant_to_Aging_Services_Technologies_HR_3590.pdf. Last accessed: September 29, 2015.
54. McGuinness, D. The Lean Post (2013). No Really, Go to the Gemba. Available online at:https://www.lean.org/LeanPost/Posting.cfm?LeanPostId=65. Last accessed: July 29, 2015.
55. Cunningham, T. and Geller, S. Organizational Behavior Management in Health Care: Applications for Large-Scale Improvements in Patient Safety. Available online at: http://www.ahrq.gov/professionals/quality-patient-safety/patient-safety-resources/resources/advances-in-patient-safety-2/vol2/Advances-Cunningham_11.pdf. Last accessed: July 29, 2015.
56. Bowers, et al. (2007). A Practical Guide to Transformation: Implementing Change in Long-Term Care. Available online at:https://www.nhqualitycampaign.org/files/Implementation_Manual_Part_1_Attachments_1_and_2.pdf. Last accessed: July 29, 2015.
57. Collins, J.C., Porras, J.I. (1996). Building Your Company’s Vision. Available online at: https://hbr.org/1996/09/building-your-companys-vision. Last accessed: July 29, 2015.
58. Recardo, R.J. (2008). Organization Design: A Practical Methodology and Toolkit. HRD Press, Inc.
59. University of Wisconsin-Extension (1998). Strategic Thinking In-Service materials. Available online at:http://uwcc.wisc.edu/coopcare/docs/vision.pdf. Last accessed: July, 29, 2015.
60. QAPI at a Glance. Available online at: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-13-05.pdf. Last accessed: July 29, 2015.
61. CAST Strategic IT Planning Portfolio. Available online at: http://www.leadingage.org/StrategicITPlanning.aspx. Last accessed: September 29, 2015.
62. Combe, M. (2014). Change Readiness: Focusing Change Management Where it Counts. ©2014 Project Management Institute, Inc. Available online at: https://www.pmi.org/Learning/~/media/PDF/Knowledge%20Center/Focusing-Change-Management-Where-it-Counts.ashx. Last accessed: July 29, 2015.
63. Cullen, L., Adams, S.L. (2012). Planning for implementation of evidence-based practice. J Nurs Adm. Apr;42(4):222-30.
6http://644. Rantz, M., et al. Challenges of Using Quality Improvement Methods in Nursing Homes that “Need Improvement”. J Am Med Dir Assoc. 2012 October; 13(8): 732–738. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3461118/. Last accessed: August 22, 2015.
65. Guide to Implementing Quality Improvement Principles. Available online at:http://www.gmcf.org/AlliantWeb/Files/QIOFiles/Nursing%20Homes/Implementing%20QI%20Principles%2010SOW-GA-IIPC-12-237.pdf. Last accessed: July 29, 2015.
66. State of Technology in Aging Services According to Field Experts and Thought Leaders (2010). Available online at:http://hweb.leadingage.org/State_of_Technology_in_Aging_Services_According_to_Field_Experts_and_Thought_Leaders.aspx. Last accessed: July 29, 2015.
67. Aging Services Technology: Report to Congress (2012). https://aspe.hhs.gov/basic-report/report-congress-aging-services-technology-study. Last accessed: August 22, 2015.
68. Workflow Assessment for Health IT Toolkit. Available online at: http://healthit.ahrq.gov/health-it-tools-and-resources/workflow-assessment-health-it-toolkit. Last accessed July 29, 2015.
69. PMBOK® Guide Third Edition (2005). A Guide to the Project Management Body of Knowledge. Available online at:http://www.knowledgecentury.com/download/PMBOK_Guide_3rd_Edition_13July2005.pdf. Last accessed: July 29, 2015.
70. QAPI Communications for any organization for any component of QAPI, such as performance improvement objectives. http://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/QAPI/downloads/CommunPlan.pdf. Last accessed: July 29, 2015.
71. Doran, G. T. (1981). “There’s a S.M.A.R.T. Way to Write Management’s Goals and Objectives”, Management Review, Vol. 70, Issue 11, pp. 35-36.
72. QAPI Goal Setting Worksheet. Available online at: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/QAPI/downloads/QAPIGoalSetting.pdf. Last accessed: July 29, 2015.
73. QAPI Measure/Indicator Collection and Monitoring Plan. Available online at: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/QAPI/downloads/MeasIndCollectMtrPlandebedits.pdf. Last accessed: July 29, 2015.
74. QAPI Measure Development Sheet. Available online at: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/QAPI/downloads/MeasIndicatDevWksdebedits.pdf. Last accessed: July 29, 2015.