Creating a Staff-Centered Workplace: Lessons Learned from Person-Directed Care
Home » Creating a Staff-Centered Workplace: Lessons Learned from Person-Directed Care
The aging services sector is always changing—new regulations, new best practices, new models of care—aging services leaders have become experts in adaptation. Yet there is one crisis that continues to stump our sector, and that is the workforce crisis.
The demographic shift has been anticipated since the baby boomer generation was born, and the last two years of the COVID-19 pandemic expedited the workforce pressures we long anticipated. Yet decades worth of underfunding, layered regulation, punitive environments, and low societal perception of aging in general has created organizational cultures that are challenging to elevate.
Still, aging services leaders are experts in culture change. For the past 25+ years, leaders have transformed care delivery models from provider-directed institutions to person-directed communities through the culture change movement. Providers had the opportunity to envision and enact a new model of care that at one time seemed impossible: One that honored the individual, offered choice, elevated dignity and respect, and turned institutions into homes. The Pioneer Network was one of the national drivers behind this change, with a primary goal of initiating “care and support [that is] person-directed, not system-directed… where flexibility and self-determination are embraced and practiced.” The continuum of culture change, as noted below, ends in older adults experiencing citizenship, where they have influence, the ability to solve problems, share responsibility, contribute, exercise autonomy, connection, and well-being.
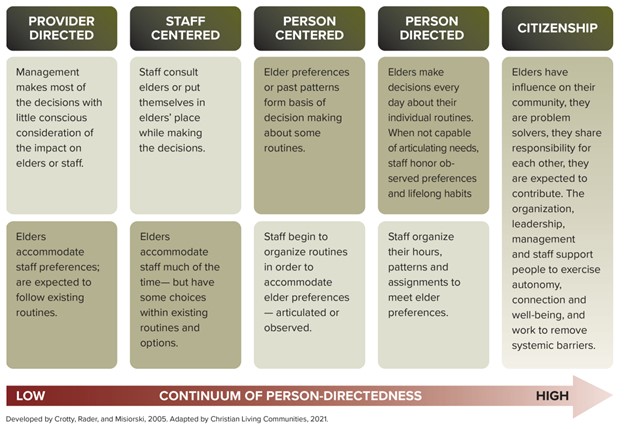
So what if we took the lessons learned from person-directed care and adapted them for our work environments? Afterall, don’t staff also want to have influence, the ability to solve problems, share responsibility, contribute, exercise autonomy, connection, and well-being?
Organizational culture change is a multi-faceted approach, supported by all levels within the organization, and integrated into the system and procedures. Creating a staff-centered workplace is about respecting, listening to and supporting staff, open communication and feedback, coaching and mentoring, empowering staff, integrating staff at all levels into decision-making, teambuilding, and cultural competence. Organizations need to build a foundation of a inclusion and respect, embedding these values in the structure, systems, policies, procedures, budgets, and strategic plans.
What if staff were empowered to solve problems, share responsibility, contribute to the team, and exercise autonomy?
Caregivers who are on teams with decision-making authority are decidedly more effective. Research shows that empowered nursing assistants in LTSS have better attitudes, performance, efficiency, and retention. One study found that empowered nursing assistants “felt that their jobs were more worthwhile and that they were making a difference in the residents’ lives,” (Splete, H., 2008). This impact reached beyond nursing assistants to nurses, as nurses who work with empowered nursing assistants were themselves happier and more likely to remain employed. As it turns out, when nurses can trust and rely upon their team members, they are more engaged and satisfied at work too. And the cherry on top? Quality of care sees marked improvement as well.
We see examples of this in the hospitality world as well. The Ritz Carlton is well known for empowering staff at all levels to exercise autonomy in addressing customer concerns, with significant power to resolve customer problems without asking permission from their supervisor. In fact, every staff member (including housekeeping) is authorized up to $2,000 to resolve customer concerns without their supervisor’s approval. The hotel company notes that employees rarely come even close to that amount, but the authority and autonomy allows them to be creative and effective in resolving customer needs with immediacy. Staff are trained well and trusted fully, and that ability to solve problems at the frontline can catapult an organization forward when given the opportunity.
From a workforce perspective, many organizations are stuck at the “Provider-Directed” level on the Continuum of Person-Directedness model, where management makes most decisions with little consideration of impact on staff. What steps can organizations take to begin to change the hierarchical structures?
Ideas to empower caregivers:
- Include caregivers in interdisciplinary teams
- Include caregivers in care conferences
- Allow caregivers to lead or inform special projects
- Include caregivers in stand-up meetings
- Teach caregivers continuous quality improvement methods and allow them to take on QI projects
- Solicit caregiver input when developing new initiatives or in providing influence on organizational decisions
- Allow caregivers to find and implement their own solutions to their own challenges
- Encourage and entrust caregivers with resolving the concerns of the older adults you serve
What if staff felt connection and well-being at work?
A 2018 Gallup poll found that having friends at work has a significant impact on connection and well-being within an organization. Staff who have a best friend at work are seven times more likely to be engaged employees, produce higher quality work, have a greater sense of well-being and commitment to the organization. Further research indicates that friends who work together are more likely to communicate successfully, encourage one another, and commit to their work, decreasing their intent to leave and increasing overall satisfaction.
With employee turnover at an all-time high, and social-isolation a new buzzword thanks to COVID-19 related quarantines, workplace friendships are all the more important. The LTSS Center’s Feeling Valued Because They Are Valued report notes that caregivers must be respected and appreciated by their employers, which requires deliberate and systemic approaches. It’s beyond fluff – workplace relationships and connections are the glue that keep our staff engaged. The importance of communication and support was further validated by the LTSS Center’s report on COVID-19: Stress, Challenges, and Job Resignation in Aging Services research, which demonstrated providers can mitigate stress felt by caregivers when they provide quality staff communication, support for mental well-being, and wrap around services.
Ideas to facilitate connection and well-being:
- Implement mentor programs so that new employees have an immediate connection, someone to turn to, and someone to sit with at lunch
- Invest in addressing diversity, equity, and inclusion
- Encourage and facilitate conversation and host activities that cultivate a spirit of fun. When peers have an opportunity to build relationships beyond superficial chit-chat, it builds camaraderie and vulnerability between colleagues
- Build teams: solving problems together creates a shared experience, joint sense of accomplishment, and builds trust amongst colleagues
- Focus on leadership skills for frontline managers through trainings such as Nurse LEAD or Geri Res
- Develop strong systems for communication, such as stand-up meetings, town halls, one-on-one meetings, electronic messaging, etc.
- Get to know individual staff members and what they need in their personal and professional lives. Develop clear structures to hear from staff, and concrete systems for following up on staff recommendations
Turning care plans into development plans
Another key feature of person-directed care is having a detailed care or service plan that honors preferences, lifelong habits, and self-determination, which is typically updated as directed by the older adult and their care team during care conferences or per a change of condition. Similarly, organizations should implement Individual Development Plans (IDPs) to ensure staff are receiving the coaching and support they need to grow in way that honors the preferences, expertise, and career trajectory of the staff member. IDPs should be updated once or twice a year, or as needed as a staff member completes education or goals.
These plans are co-written between staff and their supervisors during one-on-one conversations and can lead to engaged staff who feel supported and encouraged by their manager. When IDPs are developed and put into action, staff grow their skills and organizations see engaged, dedicated, and empowered team members. For these plans to work, the staff member, supervisor, and organization leadership need to be fully committed to the individual development process and the power behind fully supporting the goals and vision of individual team members. An organization that offers IDPs without full support risks disengagement of the team members involved. Rather than a superior-subordinate relationship, IDPs require a supervisor who sees themselves as a coach or mentor.
Ideas for professional development
- Attend a training, a conference, or enroll in an online course
- Read a book in a key subject matter area
- Participate in or lead a new project to build a specific skill
- Participate in or lead a quality improvement initiative
- Lead or participate in a committee or task force
- Engage with a local or LeadingAge committee or affinity group
- Job shadow, conduct an informational interview, or meet with the CEO
- Assist or job shadow in another department
- Connect with peers in another organization
- Become a peer mentor or a reverse mentor
- Take on a new responsibility
Transforming the workplace
Transforming organizations from an institutional medical model to person-directed care was a significant change in practice and took decades of commitment to accomplish. It took innovation, dedicated leaders, and risk. It took setbacks, laser focus, and not giving into ‘the way we’ve always done it.’ Transforming organizations from a hierarchical workplace model to a staff-centered model is no different. It is important to ensure the policies and practices reflect these values, so they are used by all staff, and to ensure there is an accountability process. Organizations need to continuously evaluate the systems and structures for a positive workplace culture.
Leaders need to stay strong in their vision, believe in the power of citizenship, and continue to value and intentionally support individuals. Our ability to recruit, retain, and build healthy workplace cultures that thrive in the future depend upon it.
Resources
- https://www.caringfortheages.com/article/S1526-4114(08)60140-7/fulltext
- https://journals.sagepub.com/doi/abs/10.1177/0733464816665204
- https://psycnet.apa.org/record/1997-03701-006
- https://hbr.org/2022/10/the-power-of-work-friends
- https://hbr.org/2017/08/having-work-friends-can-be-tricky-but-its-worth-it
- https://www.dol.gov/sites/dolgov/files/odep/topics/youth/softskills/teamwork.pdf
- https://leadingage.org/wp-content/uploads/drupal/Workforce%20Individual%20Development%20Plan.pdf
- https://www.ltsscenter.org/covid-19-in-nursing-homes-who-is-leaving-the-job/
- https://journals.sagepub.com/doi/10.1177/07334648211040509

Most Recommended
October 15, 2025
 Shutdown Week Three: Impact of Ongoing Closure on Affordable Housing
Shutdown Week Three: Impact of Ongoing Closure on Affordable Housing
February 14, 2026
Fiscal Year (FY) Funding 2026
October 07, 2025
Immigrant Workforce Matching Program Brings Workforce Relief
Recently Added
February 20, 2026
House Passes Housing for the 21st Century Act
February 20, 2026
HUD Proposes Immigration Eligibility Changes for "Mixed Status" Families
February 20, 2026
TPS Terminations: LeadingAge Explains Member Impact To Congress
February 18, 2026



