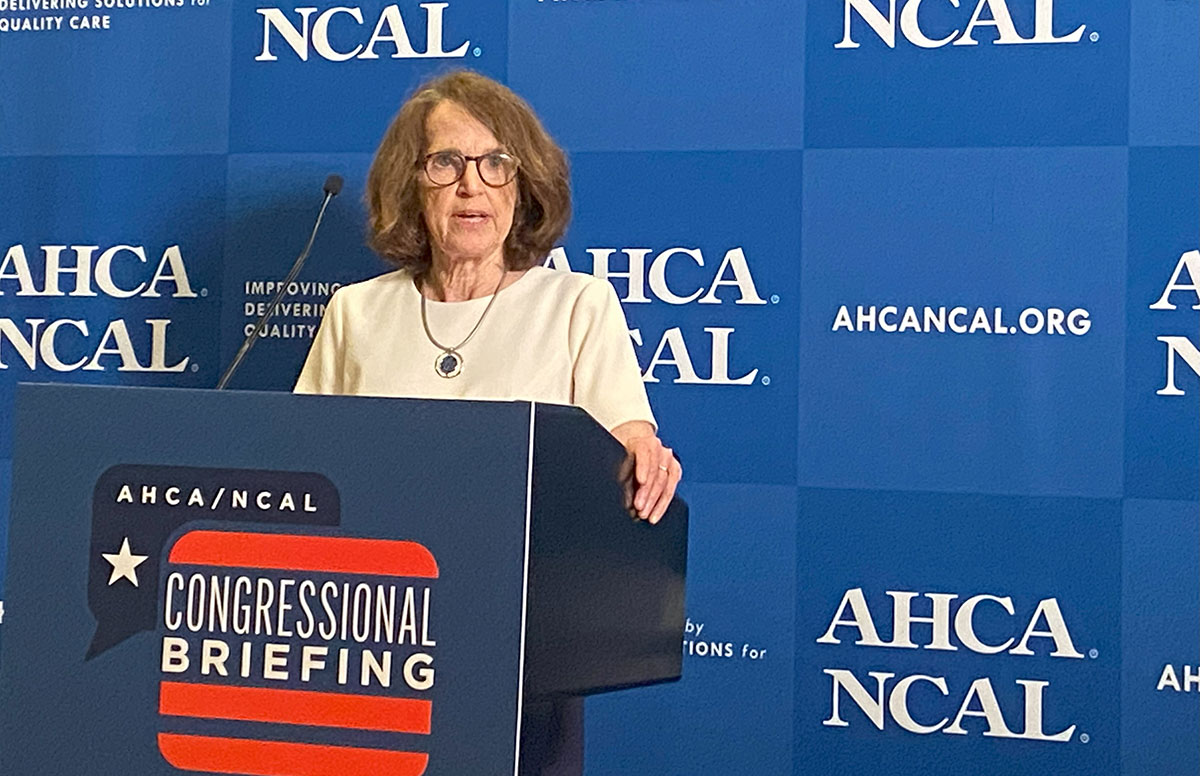
LeadingAge president and CEO Katie Smith Sloan this morning joined long-term care associations as well as nursing home providers to explain why the Centers for Medicare and Medicaid Services’ (CMS) final nursing home staffing rule must not be implemented and policymakers must shift focus to support policies that will ensure funding and support for the long-term care workforce.
Speaking at a press event alongside leaders from the American Health Care Association (AHCA), the National Rural Health Association, National Association of State Veterans Homes, and providers including Good Samaritan Society, Sloan emphasized the commitment of LeadingAge’s nonprofit and mission driven provider members—many of whom have served their communities for decades and even more than a century—to ensure quality care in nursing homes: “We know, deeply, the essence of caregiving. We fully share the Biden Administration’s goal. At the same time, we have made clear that our current infrastructure of long-term care cannot sustain staffing mandates until they are supported by adequate funding and available staff,” she said. LeadingAge decided to join with AHCA in its lawsuit to stop the mandate because, as per this June 4 press release, it does “not acknowledge the interdependence of funding, care, staffing, and quality.”
Workforce-related challenges, Sloan shared with the audience, continue to force members to regularly make hard choices, such as paring back admissions and taking beds off line: A rural Connecticut has reduced census from 91 beds to 65….. 26 people in need of nursing home care who won’t be served by that community. Or, consider our Rhode Island member, she said, that, despite deploying several schemes to maintain operations—residents and staff even held a bake sale to raise funds—announced plans to close next month. In Maine, the state with the oldest population in the country, 40% of nursing homes have already closed.
Sloan urged policymakers to shift their focus from mandates to solving the current and growing challenges in access to care: “what we should ALL be concerned about is the lack of access to services when they are needed” and the urgency to address workforce challenges. There are “back ups in hospitals because patients cannot be discharged due to lack of caregivers, because there are not available home health services or nursing home beds.”
Direct care workers—nurse aides—are critical to home health, to hospice, to assisted living, as are registered nurses and LPNs, Sloan said; with existing supply already limited, the mandate will create intense workforce competition between post acute care providers and hospitals. “We must also consider workforce supply. We have a math problem—supply and demand are far out of line.”
Sloan wrapped her remarks outlining LeadingAge’s approach: “Real policy solutions and investments, not mandates, are needed. We are drawing on every available tool—legislative, legal, and regulatory—to stop this rule’s implementation and to address the fundamental issue of building the long-term care workforce.” Policy actions to address this sector’s issues include:
- Align reimbursement to the actual cost of care, including paying staff a living wage.
- Support education and training: These are highly specialized jobs that need to be supported through ongoing education and training, including aligning federal and state training requirements and lifting limits on clinical training sites.
- Fix our immigration system to allow more foreign-born workers to come to the United States.
Bottom line, Sloan said: “We need to stop the mandate and address long-term care workforce needs.”
 Shutdown Week Three: Impact of Ongoing Closure on Affordable Housing
Shutdown Week Three: Impact of Ongoing Closure on Affordable Housing Colleagues on the Move, March 4, 2026
Colleagues on the Move, March 4, 2026


