One of the main reasons providers find it difficult to recruit and retain direct care staff is that wages are generally low, despite the demanding nature of work. Low wage rates have made it difficult for many long-term care providers to compete with other employers who can offer workers less physically- and emotionally demanding jobs. Here we have examined the different approaches state legislatures have used in recent years to increase wages. This overview includes state examples to illustrate the approaches; it is not a complete description of activities in every state.
ARPA Funds. Federal funds during the COVID pandemic became a temporary lifeline for many providers to retain and recruit direct care workers. Some states are continuing to use those funds to temporarily increase wages, while others are making the temporary changes permanent. A good example is Colorado using ARPA funds to increase rates for Medicaid home and community services (HCBS) providers to pay their direct caregivers a base wage of $15, up from the current state minimum wage of $12.56. The state’s budget for 2022-23 includes funding to make this raise permanent. Earlier in 2022, the legislature also passed a bill to increase the minimum wage for Medicaid nursing facility workers to $15 per hour.
States that continue to use ARPA and CARES act funds to temporarily increase wages for direct care workers include Iowa and Ohio. They don’t have provisions yet to make the temporary changes permanent.
Ohio appropriated $300 million in federal pandemic relief funding for nursing homes. Funds cannot be used for staff agency labor costs, or for executive, owner, or administrative pay; however, according to the legislation, the $300 million is reserved for the pay, bonuses and incentives to recruit and retain the state’s direct care workforce. In addition to $300 million for nursing homes, the bill sets aside $23 million for hospice services and $33 million for assisted living facilities, providers that have also experienced severe staffing shortages during the pandemic. The Ohio Department of Medicaid (ODM) will be responsible for distributing the money. ODM plans to allocate the money based on each skilled nursing facilities (SNF) certified bed count as of December 31, 2021.
Iowa appropriated rate increases of $14.6 million for the HCBS waivers as part of the American Rescue Plan Act (ARPA). The entire rate increase must be used for wages and associated costs specifically for direct support workers and frontline management. ARPA funds in the HHS budget will be used to prop up increases in the Iowa budget through 2024. According to Iowa Human Services, the average pay for direct-care workers is about $13 per hour; these extra funds would raise that to $16 per hour.
Commissions. In compliance with the Workforce Innovation and Opportunity Act (WIOA), all states have a statewide workforce development board or council, and these groups of community leaders are charged with planning and oversight for workforce programs and services in their area. These councils are often convened by the Department of Labor. In recent years, some state legislatures have established additional formal commissions to address the workforce crisis in long term care. The purpose of these commissions is to work with key stakeholders to understand the core issue and provide viable recommendations to the decision-making authority. Maine’s Commission to Study Long Term Care Workforce Issues submitted a report on its findings and recommendations to the Joint Standing Committee on Health and Human Services. The recommendations included (but were not limited to) increasing wages for direct care workers to no less than 125% of the minimum wage. As a result of this study, in 2021, Maine’s Governor announced $7.6 million in the state budget for paying direct care workers to align with the wage recommendation. The change will be effective this year.
Maryland is also doing a similar study focusing on strategies to reduce turnover in LTC by emphasizing wage increases. The commission consists of the Governor, members of the assembly, state agencies, educational institutions, and community providers. The final report on the findings and recommendations is due on December 31, 2023, to the Senate Education, Health, and Environmental Affairs Committee and to the House Health and Government Operations Committee. LeadingAge will be monitoring this to see what recommendations they present.
Minimum wage. States are choosing to mandate a distinct minimum wage for direct care workers. For example:
- California has set the minimum wage at $15 per hour for businesses with over 26 employees. However, in June 2022, the Los Angeles Mayor signed an ordinance into law which raises the minimum wage for healthcare workers to $25 per hour at institutions including hospitals, doctor groups, affiliated clinics and nursing facilities. The rate would be adjusted annually for the cost of living starting on January 1, 2024. The wage rate was scheduled to go into effect in August 2022.
- North Carolina increased the hourly wages for direct care workers to $15 per hour from the then-current rate of $7.25 per hour. The rate applies to HCBS workers under the HCBS waiver and was effective on March 1, 2022. This legislation appropriated $210 million to begin moving worker wages toward a minimum of $15 per hour during the 2022 state fiscal year. The rate increases are intended to be permanent.
- Washington state has allocated close to $48 million in the 2023 state budget to target wage increases for certain job categories. The intent is to provide Medicaid funding to raise wages for some of the lowest-paid jobs in nursing facilities; these include direct care (DC) and indirect care (IDC) staff (dietary, laundry, medical assistant; IDC- housekeeping, reception, transportation, etc.) This is accomplished by raising the DC and IDC medians, respectively, from 105% to 111% for DC and from 90% to 92% for IDC. The Department of Social and Health Services (DSHS) is directed to work with stakeholders to develop a verification process to demonstrate how providers will use this increased funding to increase the targeted wages.
Wages based on years of experience. Several states are raising the minimum wage for direct care workers to a living wage. Although a step in the right direction, it can create a difficult pathway for the rest of the wage scale because of wage compression.
To address this issue, Illinois created a pay scale for direct care workers based on years of experience and the promotion of career ladders. Governor Pritzker signed legislation that will invest more than $700 million in Medicaid funding for nursing home rate reform. The reform principles include (but are not limited to) a new pay scale for certified nursing assistants (CNA) that will increase wages based on years of experience. This legislation created the CNA incentive program, an optional program in which participating nursing facilities can receive funds subsidized by Medicaid if they implement the CNA experience pay scale. For CNAs with at least one year of experience, their wage will increase by at least $1.50 per hour. The pay increase goes up by $1 for each year of experience and tops out at a $6.50 per hour increase for those with six or more years of nursing experience. In additional to years of experience, Medicaid will also subsidize CNA raises for promotions or added duties at a rate of an additional $1.50 per hour.
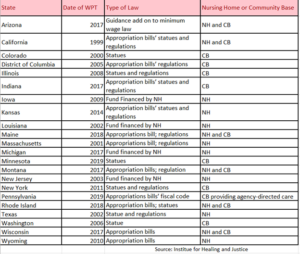
Wage Pass Through (WPT): Faced with significant shortages of direct-care workers in long-term care, 22 states have enacted wage pass-through provisions as part of their Medicaid programs. States adopting a wage pass-through policy require that a certain portion of the Medicaid reimbursement increase be devoted to staffing through raises to direct-care wages. The table below summarizes enacted state wage pass-through legislation.
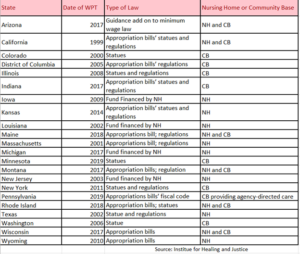
Two methods are commonly used by states to calculate the amount to be allocated for wage pass-through programs. The first is to identify a set dollar-amount to increase worker wages “per hour” or “per patient-day “within the Medicaid reimbursement rate. The second is to require that providers spend a percentage of a specific rate increase on higher compensation. For each provider group, states can either establish a single payment rate or set different amounts, determined by size of the facility, acuity of patient mix, ownership, geography, or other criteria (HHS, ASPE) .
The challenge with the WPT is that little is known about its effectiveness in achieving the intended goals to boost direct care staffing and reduce vacancies and turnover. The accountability measures also vary from state to state. Some states have no clear measures while others are required to submit a certification of compliance annually.
Wages directly to workers. In contrast to reimbursing through Medicaid, some states are enacting a much more direct approach, by putting the dollars directly in the hands of the direct care workers.
Connecticut established the “Connecticut Premium Pay program” to provide $200 to $1,000 to essential workers who were providing health- and childcare services throughout the pandemic. To be eligible, workers must have earned $150,000 or less, and must have worked in the private sector (federal, state, and municipal workers are not eligible.) The program recognizes and compensates these dedicated workers for their service. A total of $30 million was allocated for the program in the 2022 state budget. There are close to 53,000 workers and each must apply individually by October 1, 2022.
Recently, New York announced $1.2 billion for the Worker Bonus Program (HWB) aimed at rewarding and retaining frontline health care and mental hygiene workers. Passed as part of the state budget, this program requires health care providers to pay up to $3,000 in bonuses to health care and mental hygiene practitioners, technicians, assistants, support staff, and aides. Qualified employers are employers that bill under the state Medicaid plan, the home and community-based services (HCBS) waiver, or Medicaid through a managed care organization or managed long term care plan. Employees must be receiving an annualized base salary (excluding any bonuses or overtime pay) of $125,000 or less, and can be full-time, part-time, or temporary. Bonuses for employees will be determined by hours worked during a consecutive six-month period between October 1, 2021, and March 31, 2024. Eligible employers can submit employees who qualify for HWB payments by creating an account on the online HWB portal.
The LTC workforce crisis is an ongoing problem. There is no one size fits all solution to this. It Is a positive sign that state legislatures are recognizing the workforce crisis and taking steps to address this issue. However, it is not clear which of these approaches will be successful in recruiting and retaining the direct care workforce. LeadingAge will continue to track trends and innovative approaches out of the state legislature. Updates will be made as new information becomes available.

 Shutdown Week Three: Impact of Ongoing Closure on Affordable Housing
Shutdown Week Three: Impact of Ongoing Closure on Affordable Housing